Prolapse is often considered a very scary diagnosis because it is talking about the center of our femininity and it’s often diagnosed on the heels of bringing life into the world. I think that’s the part that makes this diagnosis so hard. You’re now a sleep-deprived mother working hard to keep a little one alive and happy, and this is what you get? (Just being real with feelings here.)
Let’s shed a little light on it so it’s not so scary or devastating and see how we can make improvements that don’t require surgery, just some good ol’ fashion hard work.
I’m in the business of rehab, not surgery, so I’m going to dive into what the non-surgery path looks like for prolapse. There is room for hope. I’ve seen a lot of women with prolapse improve. Some women heal completely, some improve by a grade or two, others are able to master movement and do anything they love, including running and jumping, without fear of making their prolapse worse. Some of that depends on determination and some of it is genetics. I don’t know where your recovery ceiling is but I do know that if you don’t give it your all, you’ll never find out.
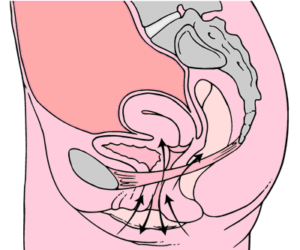
When you think of the word prolapse, you think of something coming out. It’s prolapsing. So pelvic organ prolapse is the organ(s) descending down into the pelvic cavity from where they should be sitting.
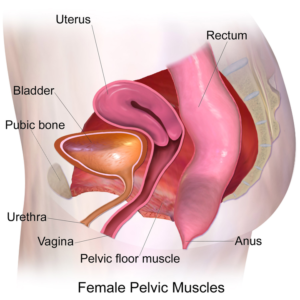
Typical Location of Pelvic Organs
Some prolapse postpartum can be completely normal. Yep, I said normal. Normal amounts of prolapse followed by correct movements create a healing environment. Some experts believe that almost 100% of women have some level of prolapse immediately postpartum and that “a little give” in the pelvic organs is completely normal following delivery.
Many women never even know they had a prolapse postpartum but the percentage is high, up to 50%. Minor prolapses often go unnoticed until they become something more. Changing patterns can keep a minor prolapse minor or even improve it, which makes me wonder why we aren’t having these conversations earlier in the process!
You don’t have to have a baby either to end up with prolapse. Poor pressure management when lifting or chronic coughing combined with pelvic floor muscle weakness can be enough to cause prolapse.
If you’re one of the “lucky” ones who ends up with a bit more than normal or minor prolapse, it’s going to take a bit more extra effort to help it improve. (I was one of those lucky ones, which is why I get to write from both first-hand knowledge and clinical knowledge.)
Prolapse is caused by a combination of several things. Understanding that combo helps you attack the treatment. Let’s look at three main contributing factors:
1. Ligament and tissue laxity. This is very common postpartum due to the laxity needed to stretch for pregnancy, prepare for delivery, and the stretching of delivery itself. This is where genetics comes into play. Some women have more reboundy tissues than others due to their genes. But don’t discount diet here! A nutritious diet with good hydration can help with tissue quality and repair, a great reason to feed your body well. I’ve seen that tissue laxity can improve over time, but it takes a long time!! I’ve even seen women have improvements in tissue laxity years after having a baby. Breastfeeding can make us hang on to that laxity, but I don’t think worrying about laxity is a reason to stop breastfeeding. All things come in time, and rushing that one probably won’t change your end result at all since there are so many other factors that you can be working on.
This is also why so many women notice prolapse when they hit menopause. Our hormones play a role in our tissues. There are a few options that help with this. Building strength, managing pressure and then talking to your doctor about vaginal estrogen can help.
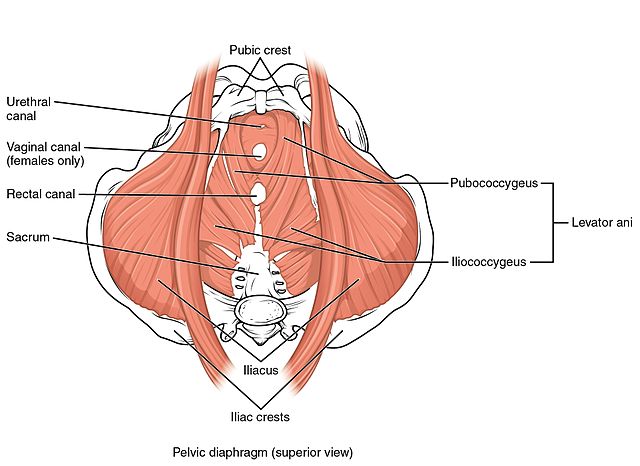
2. Muscle weakness. Our pelvic floor muscles support our organs. If those muscles are weak, it makes organ support difficult. Sometimes this is where kegels or pelvic floor contractions come in. Other times women just need to work on alignment of their ribcage, thoracic spine, head, or hips in the socket and the pelvic floor muscles “magically” get stronger, no kegels needed. This is very true if you’ve been “doing your kegels” and you’re not getting stronger. This means your strength issue isn’t coming from your pelvic floor, your pelvic floor is just feeling the results of poor alignment.
Some women need kegels to build strength, and some women tend to naturally tighten all the time. If you fall into the naturally tighten all the time group, kegels will probably make you worse AND your prolapse symptoms might be caused completely by the tightness.
This prolapsed appearance and symptoms are being increased or completely caused by the tightness. Think about an accordion. Picture the folds when you bring it together. When the pelvic floor muscles are tight, imagine them looking a lot like an accordion. You get bulging tissue that looks and feels a lot like a low grade prolapse. If you’re wondering why your symptoms come and go so dramatically, it might be tightness. Now picture lengthening the accordion out, see how it stretches the walls and they now no longer look bulgy?
I notice that women can get stuck in a fear cycle though, where they hold their PF tight because they feel the “prolapse” which in turn makes the prolapse worse and decreases the pelvic floor’s ability to work. Over time this tightness creates pelvic floor weakness, and weakness can lend itself to worsening prolapse. So learning to relax and then strengthen is very helpful!
Sometimes your prolapse will look worse once you learn how to relax. This is normal and fine, that just means it’s time to build some muscle and work on getting stronger, but at least you’re now at a better starting point.
Ok, back to muscular strength. When muscles get stronger, they bulk up. Think about that big bulky guy at the gym with lots of muscles. 🙂 This bulking or increasing muscular thickness and strength helps in two ways.
-
- It helps you handle increased pressure from things like coughing, sneezing, bearing down when you lift, and gravity during jumping. Those muscles work hard to keep your organs in place. The more muscle you have, the more you are able to hold things up

2. The thickness itself can fill in for tissue laxity. As the baby goes through the vaginal canal, tissue gets stretched. Think about saggy skin. The more volume you have taking up space, the less sag. Think about your stomach. Newly postpartum you probably didn’t realize how much stretched out skin you had, but then when you lost weight, you noticed more loose skin. When you add bulk to muscle, this helps with support. We want really strong pelvic floor muscles. Weakness is actually one of the leading causes of prolapse surgery failure rates. Just something to ponder…
I know what you’re thinking, “Ok, Sarah, in a perfect world this sounds great, but I had severe tearing during delivery and am missing some of my pelvic floor muscle. What do I do then? I can only strengthen so much.”
I think this is important to talk about because many women experience levator ani or other muscular tearing during delivery and they don’t find out about it until they get diagnosed with prolapse. If you can catch it early, there may be a chance of being able to repair the tissue surgically and get a viable muscle contraction again. (I’m not talking about a prolapse repair here, I’m talking about reattaching the pelvic floor muscle torn during delivery.)
This type of muscle tearing is deep, not the stitching you get on the surface. So it’s often missed. A good Pelvic Floor Physical Therapist can usually catch it or at least suspect it and send you in for further imaging. So if you suspect that your pelvic floor contraction feels a lot weaker than it did before delivery, it’s worth a session with someone good to find out for sure. That way you can get advice and weigh what your next steps might be.
What if you’re past the window for a surgical repair, don’t want surgery, or only have a partial tear? There are a couple of things that I’d really like for you to keep in mind.
- You have lots of muscles in the pelvic floor. So other muscles can help pick up the slack. Strengthening is still and always will be a good idea!
- Be a pressure management ninja. Because you’re a little more vulnerable to prolapse, you’ll need to be vigilant about bearing down. Most of the women I work with don’t realize they are bearing down (increasing pressure) during daily life. It takes lots of awareness to build better patterns.
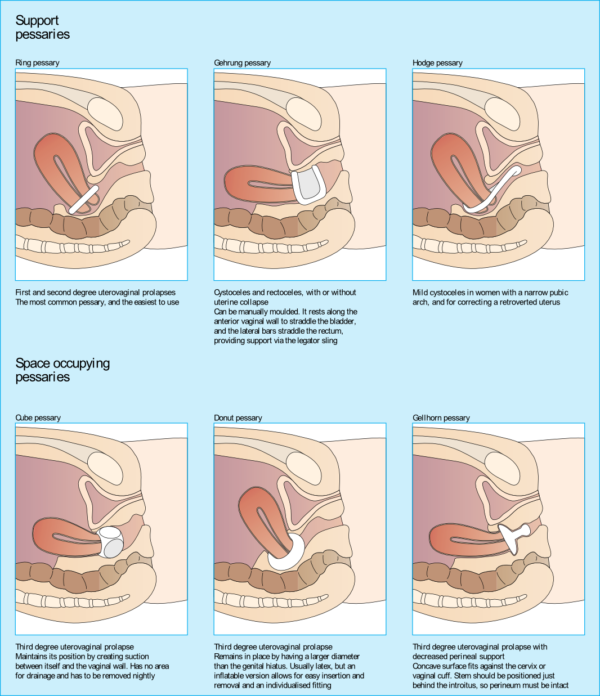
- Consider wearing a pessary for support when you know you’re going to be doing something hard. If you’re going to be distracted and overloading your body, whether that’s moving day or maxing out at the gym, it might be a good idea to give your pelvic floor a little more support. I’m generally not a fan of pessaries for normal workouts because you should be able to feel what’s happening and prevent all bearing down to improve how your pelvic floor functions in life with each workout, but in this case, it can be good. It also might take some work to get to this point though… I know things aren’t always perfect. (The other time a pessary can be the most useful is in the early stages postpartum.)
3. Pressure management. Just like you can out-eat any amount of exercise when it comes to dieting, you can out-pressure any amount of pelvic floor strength.
So, what is pressure and how do you decrease it?
Intra-abdominal pressure is the pressure created when you brace your abs. You brace for all sorts of things all day long and might not realize it. You brace to lift something, push a stroller, or yell at the internet company over the phone. I joke, but I figured out that I actually created more pressure down when I was mad and on the phone with Comcast than I did lifting weights! It’s often the times that we are the least mindful and don’t realize we are over-bracing or bearing down.
Trying to get a kid in the carseat is another common time. You have to lift and then place at an awkward angle. Sure, my three year old can get in his own carseat, but only after he’s turned on the dome light, grabbed a toy off the floor and tried to poke his sister. It’s much easier for me to just throw him in which means I need to be strong enough to lift, twist and bend without bearing down! That means I have to be strong. Everyone with prolapse should be getting stronger and lifting weights!! If not, you’ll get weaker over time. Getting weaker means you bear down or brace more, which means your prolapse gets worse. Being strong is your friend. You just have to do it safely! Expert guidance can help!!
Decreasing pressure comes with improving body awareness. You have to connect and feel. It’s really that simple, but also that hard.
Pressure isn’t all bad. Our pelvic floor muscles respond to pressure by tightening. So increasing the amount of pressure your pelvic floor has to handle over time can be amazing for strength gains and prolapse recovery. Things like an unmanaged chronic cough over time can be really hard on the pelvic floor because it’s repeated unregulated pressure down. Pressure through exercise that’s challenging yet not too much can be a really good thing. The body thrives on challenge, not lying on the couch!
Let’s dive into the different types of prolapse along with a few tips for each! Because I bet you’re thinking, does this actually pertain to me? I have a more difficult kind of prolapse.
Before we talk about the specific vaginal prolapses and different tips to target them, I want to reiterate how pelvic floor rehab of prolapse is a whole-body issue!! From posture and breathing to your arch strength, it all plays a role. So doing kegels and getting your pelvic floor stronger can help, but that’s only one part of the picture.
Free Pelvic Floor Educational Series
Dr. Sarah Duvall, PT, DPT, CPT and the CES Team have helped thousands of women create the strength and stability needed to overcome common and not-so-common pelvic floor issues.
Join us today for this 4-part Pelvic Floor Video Series, absolutely free.
We don't spam or give your information to any third parties. View our Terms of Use and Privacy Policy.
Having trouble signing up? Click here

Let’s start in the front! A cystocele or bladder prolapse responds really well to working on front pelvic floor strength and lower abdominal strength. Those lower abs and front pelvic floor muscles work together to help lift up the bladder. Being mindful of pressure from upper ab gripping is also critical. (kegel tutorial)
Closer to the opening of the vagina but still in the front, you can get a urethrocele. This is a prolapse of the urethra. This is a tough one because if you have any pelvic floor tightness it can get irritated very easily. The irritation is terrible. It feels like a UTI, except all the time, not just when you’re peeing. This can be challenging because you’ll have to keep tightness at bay while working on pelvic floor strength. The specific pelvic floor strength I like to focus on here is starting at the bottom up for a contraction. So, really focus on lightly closing the front of your vagina, don’t do any lifting of the vaginal muscles. Just focus on the closing part. I find a lot of women with a urethrocele tend to skip straight to the lifting part of the kegel. The only key is to be careful with how much you do, too much and you’ll get irritated again.
Tight transverse abdominal (TA) muscles can also play a role in the irritation. This isn’t a problem if you have a good 360 breathing pattern. It can be a big issue with belly breathing. Since you don’t get length to the TAs with a belly breath, the fascia in the front just expands more and more while the muscle itself stays tight. (The TAs are on our sides not the front.) I often notice some belly distention or bread-loaf appearance to the abs with a urethrocele irritation. Just some food for thoughts. Everything is connected!
Uterine prolapse is the hardest to rehab in my book because it takes both the strategies from the front and back of the pelvic floor to help lift that uterus. I have had a lot of patients successfully improve their uterine prolapse though, so even though it can take a lot of effort since you need to improve all the moving parts from posture, breathing, and core control all the way down to arches, it’s worth the work. The good news is that there are lots of boxes to check when you look at improving. I like it when there are so many factors, means there is lots of room for hope if you’ve tried one thing (like kegels) and that approach isn’t working.
Let’s head to the back next. A rectocele or prolapse of your rectum into your vagina sounds like the scariest, but I actually think it’s one of the easier prolapses to rehab. You don’t have to worry about irritating the urethra, which is really nice! So there is more room for aggressive strengthening.
Deep hip rotator tightness can be an issue for getting a good pelvic floor contraction in the back. So, much like with the urethrocele, I like to focus on barely getting a pelvic floor contraction in the back without contracting anything deeper in the glutes. I want everything right outside your sits bones to feel soft, squishy and relaxed. That’s step one! Then, work on being able to deepen your pelvic floor contraction without those deep hip muscles kicking in. You’ve got to teach your deep hip musculature to not compensate for your pelvic floor. Once you get that, it’s time to dive into increasing hip and glute strength. There are lots of big muscles back there, so as long as you’re balancing your pelvic floor contraction while increasing hip and glute strength you’ll start to feel some progress. Just be sure you don’t substitute hip and glute strength for pelvic floor strength. It needs to complement.
Bathroom habits matter for all types of prolapse. Let me say that again!! Bathroom habits matter.
If you power pee and push out pee, you’re forcing pressure down on your bladder. That’s not good! You should be able to sit, relax, and let pee come out. If you feel like you need to push, resist the urge and take a few deep breaths trying to relax further. If you still feel like you need to push, you’ll need to address your pelvic floor tightness. Having to push out pee is something that can be helped, and that in turn will help your prolapse.
If you have a rectocele, having a bowel movement can be stressful. There are several types of ways you can use your fingers to splint in your vagina while having a bowel movement to keep pressure on your fascial wall. You might need to stick fingers all the way in or you might just be able to get away with a little pressure at the opening, try using your thumb with a pinch of tissue, that might do the trick. Just don’t forget to wash your hands before and after, but I figure that goes without saying.
The amount of splinting needed will depend on the degree of prolapse and the degree of your tissue laxity. This is especially needed if you have any back pelvic floor tightness. Let’s put it in simple terms. You have this tube. On one side is a thick wall of tight muscle putting pressure on the tube. On the other side is a thin layer of fascia that might have gotten stretched out during delivery. Does it make sense now why giving the inside back wall of your vagina a little support during a bowel movement is a good idea and not something to get overly upset about? Fascia takes a long time to recover and a little support here will help it not get stretched out more and can eliminate the need for straining. So, if you feel like you have to push at all to have a bowel movement or stool wants to get stuck, give your vagina a little support.
Yes, needing to push to poop, like power peeing, is also bad. Avoiding constipation and straining at all costs is a good idea. Remember, bearing down causes prolapse! If you’re trying to improve your prolapse, it’s not a good idea to strain. A squatty potty can also be helpful for aligning the pelvis to help a bowel movement come out more easily. That could be a good investment for you.
Talk to your doctor about taking magnesium. Some fiber is good but too much fiber can actually be bad, so make sure you don’t overdo it there. Hydrate more. I find electrolytes to be very effective. Coconut water and blueberries are also great. Experiment and figure out what works for you.
Let’s talk for a brief moment on posture and pelvic tilt. Tucking puts a lot of pressure down on pelvic organs. The opposite, sticking out your bottom, increases paraspinal activation which can increase ab gripping which can increase pressure down. Whew! So working on posture is also important.
And it all starts with breathing! Breathing correctly is probably the single most important thing to work on when it comes to prolapse. Breathing can be hard because it’s not as simple as belly breathing, but I’ll leave it at that for now. 🙂 This blog post is getting a bit long. Thanks for sticking in there with me till the end.
Prolapse is not something to be afraid of, but it is something to be respected. Most cases of mild to moderate prolapse can be managed successfully and conservatively. Prolapse surgery failure rates are very high, so working on everything we talked through above is imperative, even if you’re going to have surgery. Many people give themselves prolapse again after the surgery because they failed to address these issues. Making some strides on the conservative side can go a long way toward success for every prolapse treatment option. This is important to keep in mind because sometimes prolapse surgery is the best answer and I want you to have the most successful recovery possible!
One last note on pain from prolapse.
If you’re experiencing pain, odds are it’s more from tightness than the actual prolapse. You can get some pain during sex if the uterus is low. (For obvious reasons.) Pain can come from an irritated urethra if you have more than a grade 2 since the tissue is very thin. A grade 2 or less with urethral irritation is probably just tightness, not thinned tissue.
So if you’re experiencing pain from a grade 1 or 2 prolapse, odds are it’s not the prolapse causing the pain. You’re actually experiencing pain from pelvic floor tightness and it has nothing to do with the prolapse. Well, you’re probably guarding and lifting your pelvic floor too much to help protect the prolapse which is causing the tightness, so I guess in a way the prolapse is causing the pain indirectly.
Prolapse is challenging because it’s a whole-body issue and is affected by how you move through daily life. It’s not like an ankle sprain where you can avoid walking on it. You interact for better or worse with your pelvic floor all day long. So the more you know, the more you can improve! Increasing body awareness, improving strength, and fixing movement patterns will go a long way. Having some grace and patience but extreme persistence with this healing process will carry you through.
If you are a professional that works with women, check out the Pregnancy and Postpartum Corrective Exercise Specialist Course. It is the world’s leading pregnancy and postpartum corrective exercise certification and will set you apart from the competition!
I also wanted to extend a special thank you to my mentor Dr. Jennifer Stone, DPT. You’ve been an amazing resource to help me work through all my crazy ideas when it comes to prolapse rehab. Thank you for educating PTs and helping to move women’s health forward.
Here are some prolapse recovery success stories from ladies I have worked with in case you needed some inspiration!
Related Articles
Pelvic Floor and Diastasis: What You Need to Know About Pressure Management

Join us today for this 6-part Pelvic Floor and Diastasis Video Series, absolutely free.
This course is designed for health/wellness professionals, but we encourage anyone interested in learning more about the pelvic floor and diastasis to sign up.
We don't spam or give your information to any third parties. View our Terms of Use and Privacy Policy.