Pelvic organ prolapse can feel like a devastating diagnosis for many women. Interestingly, some women have it and never know, while other women can tell if the slightest thing feels wrong in their vagina and seek help immediately. Mild to moderate prolapse is rarely ever painful, but pelvic floor issues such as tightness or a hypertonic muscle state can mimic prolapse, so these symptoms are actually the pain or discomfort from tight muscles and not the prolapse itself. The sensation of prolapse can feel like something is there, like wearing a tampon that hangs a little low.
Common complaints and sensations for moderate to mild prolapses
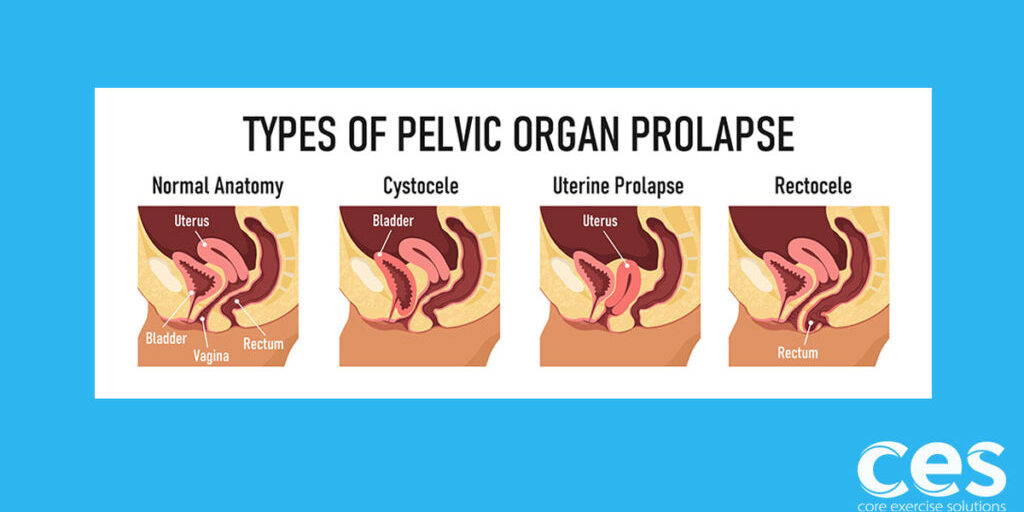
Bladder or urethral prolapse (bulge on the front vaginal wall/cystocele/urethrocele) can be associated with stress incontinence (leaking with jump/sneeze) but is usually not associated with pain or increased UTI feelings. Pain and UTI type feelings are generally caused by muscular tightness in the front of the pelvic floor and not the prolapse itself. Once the tightness decreases the symptoms usually go away, even if the prolapse is unchanged. Front prolapse can also cause some irritation during sex if the tissue has thinned out. This is more commonly seen in grades 3 to 4.
Uterine prolapse can cause some low back pain. You may also feel a “heavy” sensation.
Rectoceles (bulge on the back vaginal wall) usually don't cause any pain, but they can make having a bowel movement really annoying (lack of professional term for this!) Splinting is often recommended to ease these symptoms. This is when you place your fingers in or at the opening of the vagina and apply support to the posterior (back) vaginal wall.
All types of prolapse can cause a sensation of something being “there,” and mentally that feeling is very bothersome.
Quick note about pain and surgery:
Pain most often comes from pelvic floor muscle tightness, and surgery will not help with that -- so make sure if you’re going in for surgery, it’s for reducing the bulge and not for treating pain.
I’ve seen post-surgical patients who thought the prolapse was causing the pain, but they still had the exact same pain (or worse pain) after the prolapse repair surgery and now it was accompanied by urinary frequency they hadn’t known was an added risk.
I am very pro-surgery when it’s needed, but we just want to make sure that the surgery outcome and patient expectations match before diving into that level of treatment. I’m so glad there are surgical options and great surgeons! Healthcare has moved forward so much in this area.
A great foundation makes for a great surgery recovery! And we want to make sure someone doesn’t rush into surgery to resolve an issue that’s not being caused by the prolapse. Mild to moderate prolapses produce very few symptoms and are almost never painful.
If pelvic floor-safe strategies are not adopted, the prolapse could come back even after surgery. So, as a PT, I like getting someone to the point where their strategies are so automatic that they hardly have to think about their pelvic floor, and they know they are keeping it safe before having surgery! That’s a win that can only be gained through learning about pressure management and building strength and body awareness.
Here is a free video series that covers assessing and improving pressure management. Click here to get started.
For the purpose of this article, though, I’d like to focus on prolapse treatment without surgery. So let’s dive into more on that topic!
Prolapse Treatment Without Surgery: Can Postpartum Prolapse Heal Itself?
The human body is incredible in its ability to heal and remodel tissue. I’ve seen impressive resolution of prolapse, and I’ve also seen prolapse that remains unchanged over time. Some women have the potential to heal completely, others have the potential to heal some, and others can live life without worrying about their prolapse at all, even though the grade doesn’t change. They have learned to manage it.
Conservative prolapse treatment has several steps
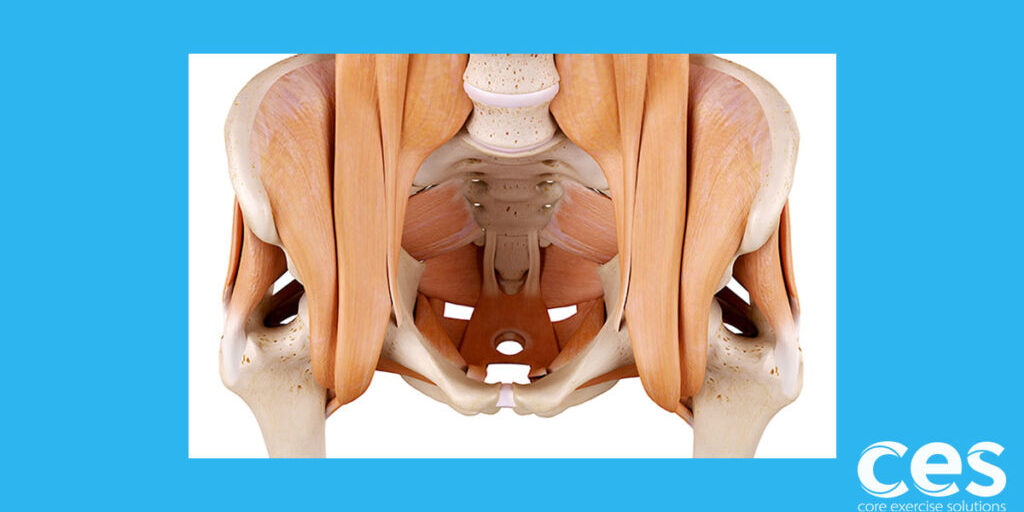
Step one: Assess the state of the pelvic floor muscles. Are they tight? Weak? Strong? What needs to happen to optimize strength? In some cases, it’s release work and relaxation. In other cases, it’s lots of kegels.
Step two: Learn how to manage pressure and bring awareness to bearing down. This includes during bowel movements, exercise, and just daily life. This is a crucial step, because you can’t out-strengthen poor pressure management. Even a super strong pelvic floor will continue to see worsening prolapse if pressure is not managed. Here is a pressure management video series with exercises designed to improve pressure control.
Step three: Strengthen the surrounding muscles. Abs, glutes, adductors, etc. Our muscular systems work together. I’ve seen women not make much progress moving through steps one and two, but when they focus on strengthening everything in a way that works with their pelvic floor, they finally start seeing results.
Keep in mind that it can take years for fascia to remodel. Seeing changes in prolapse can happen quickly for some, but for most women, it can be a much longer road. The best part of building strength and body awareness is that it’s yours to keep once you get it.
Think of it as bonus money in your health bank. It will not only improve surgery outcomes if you ever did decide to have surgery in the future, but it will help prepare your pelvic floor for menopause and aging in general. Many women notice new or worsening prolapse with menopause, so preparing for this time period can bring real, long-term health benefits.
Safe Prolapse Exercises
One of the biggest factors for improving prolapse without surgery is eliminating any exercises in your workout that cause too much pressure down on the pelvic floor.
An example of uncontrolled pressure would be lifting a heavy box, kid, or weight where you bear down to gather the “oomph” to make the lift happen. There is no magical position or weight to keep in mind, because it will be different for every person. But think of it as the point of straining, and that might be helpful.
A great example of this can be while out shopping. Pushing a cart that is too heavy can lead someone to bear down, as can picking up an awkward, full box out of the cart to put it in the trunk.
What is Pressure Management?
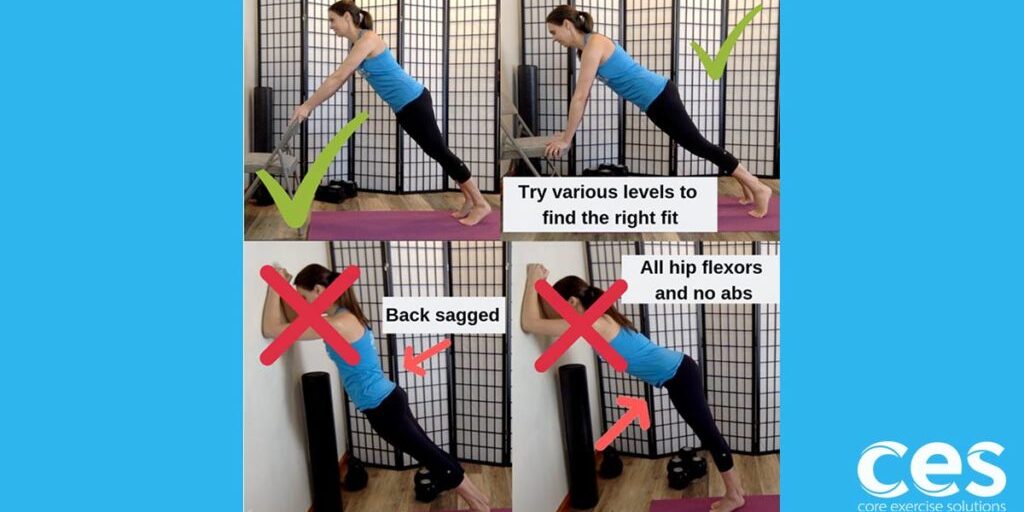
Exercise is not inherently dangerous or safe for prolapse. It’s how your body responds to that particular choice of exercise.
Squats CAN be a very safe and helpful exercise for the pelvic floor.
Lifting CAN be helpful for promoting prolapse recovery!
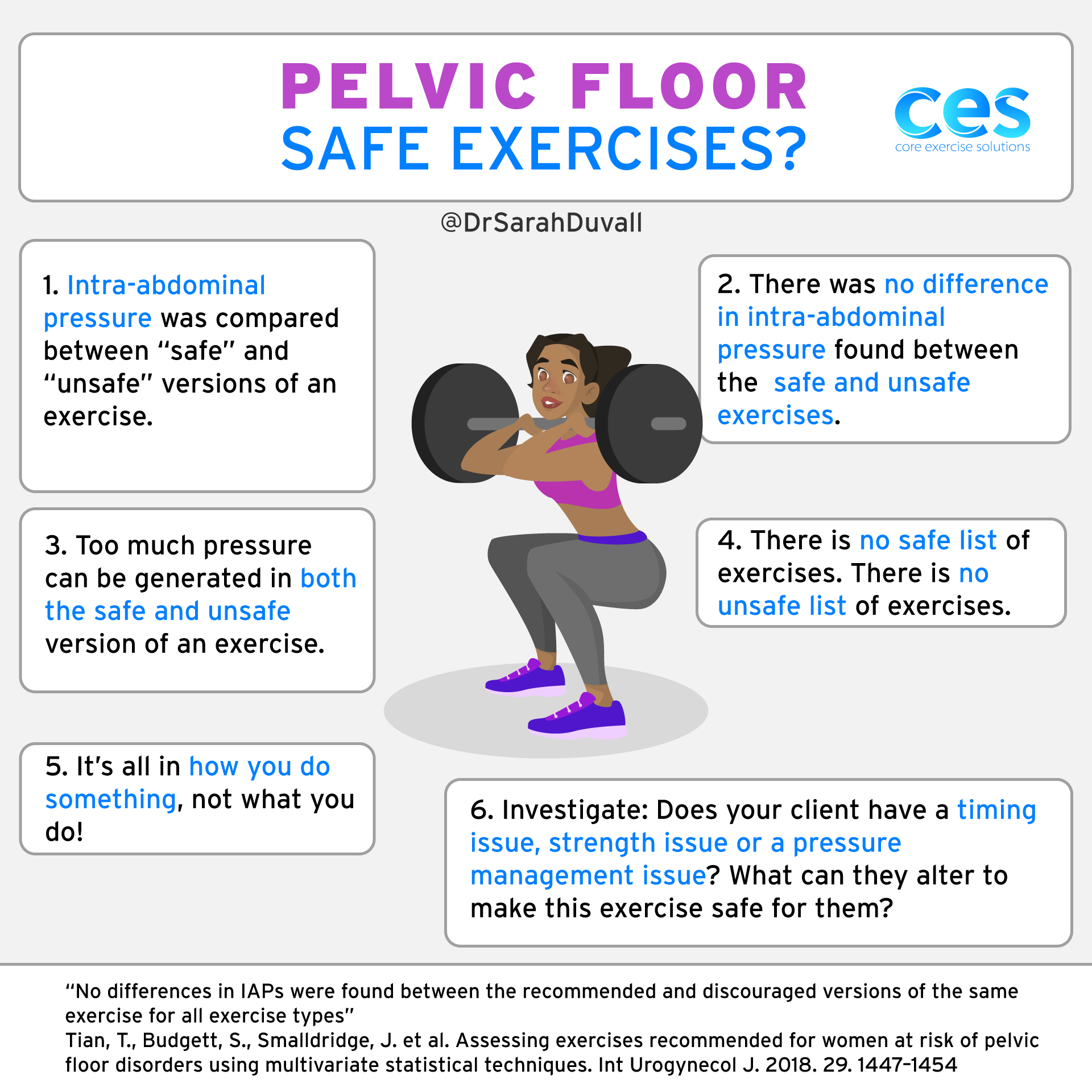
This can be very frustrating when someone wants to hear a simple list of things like, “Don’t do squats, and you won't make your prolapse worse.” If only it were that simple!
Exercises to Avoid With Prolapse
This is a very important list to generate for yourself, and it will look different from person to person.
From a clinical perspective:
- I’ve seen women who can go to their CrossFit workout and their prolapse feels amazing afterwards.
- I’ve also seen women who could go for a run if they were feeling symptomatic and it would help to resolve all their symptoms.
- On the other hand, I’ve seen women where running or heavy lifting contributed to their prolapse and made it feel worse.
- I’ve given out squats as treatment to help improve prolapse symptoms.
- I’ve also taken squats out of someone’s lifting plan because they weren’t able to manage pressure well.
- Some women have a hard time sitting at work all day, and that’s what makes their prolapse worse.
- Others can go for a run, but going to a spin class or for a swim makes them feel worse.
As you can see, “safe” is hard to define because it’s all in 𝐇𝐎𝗪 you do something, not 𝗪𝐇𝐀𝐓 you do.
I also find that just trying to live life can be much harder than exercise. Usually women are very mindful of pressure during their workout, but getting the stroller into the trunk or picking up a kid throwing a tantrum compromises their pelvic floor.
Let me give you an example of my list of things to avoid that made MY prolapse worse in the beginning.
Unsafe exercises that made MY prolapse worse (in the very beginning of my prolapse diagnosis)
#1. Carrying my heavy toddler for long periods of time when tired.
#2. Trying to hold a newborn and cook/multitask at the end of the day. (Show of hands for how many of us pulled off prepping dinner while simultaneously breastfeeding? 🙋♀️)
#3. Catching my toddler jumping off a high surface at the playground.
#4. Jogging slowly on flat ground.
#5. Pullups.
#6. Planks on the floor.
#7. Walking and pushing a stroller for longer distances while tired.
Safe exercises that made MY prolapse feel better in the beginning
#1. Sprinting uphill.
#2. Squatting and deadlifting (all lower body lifts felt great after).
#3. Walking without pushing a stroller.
#4. Heavy upper body lifting for mid back muscles (rows).
#5. Lower abdominal exercises.
This list has changed and continues to change, and so should your list! In the beginning, moving was mentally hard. I had to retrain the way my body handled pressure. It was frustrating! But also worth it!
Free Pelvic Floor and Diastasis Recti Course
What You Need to Know About Pressure Management
🎥 6 Video Lessons | 🕓 97 Min | 📑 PDF Downloads
Working with pregnant and postpartum clients/patients?
This 6-part course offers key takeaways on breathing, pelvic floor strengthening and diastasis recovery. Sign up and start learning today!
Safe Cardio Exercises for Prolapse
Why does prolapse seem to take away the one thing so many of us need to relieve stress? It’s just not fair! Cardio can be done safely, once you learn how to manage pressure. (Until then, I turned to meditation to help get that calm. Don’t hate me. LOL)
Prolapse and Swimming
- Swimming is low impact, but can be tough for someone who slips into a shallow breathing pattern, upper ab gripping, or primarily uses their hip flexors instead of their glutes for kicking force. Focusing on deep breathing, reaching and turning, as well as kicking with the glutes can help swimming feel great for prolapse. Focus on feeling your lower abs flatten as you exhale, and this will make sure you don’t bear down on those forceful exhales. The other thing that can help is to practice yelling or screaming in the car on the way to the pool and focus on what you feel happening at your pelvic floor. If you can sing at the top of your lungs without your pelvic floor bulging down, then swimming will be a lot safer. Many women also need serratus strengthening exercises to help them reach and lengthen across the pool.
Prolapse and Biking: Is Spinning Bad for the Pelvic Floor?
- Cycling is also low impact, but hunching over the handlebars or standing on the pedals to power uphill can generate a lot of pressure which can result in worsening prolapse. Working on scooping those lower abs and not over-gripping with the upper abs and keeping the resistance low enough that you don’t have to bear down to create a lot of force can help make biking a safer activity. Try raising up the handle bars and hinging forward through the hips more than hunching to relieve pressure. If you go into standing, focus on that first push into standing and aim for a nice exhale, feeling pressure leave, versus bearing down to generate that extra oomph.
Prolapse and Running
- Running can go either way. It can leave you feeling amazing, or make your prolapse feel worse. I’ve talked to women in both scenarios. The difference? Knowing your limits! And working on your running form. Running when you feel light and it feels easy seems to be much better than running when you feel heavy, or giving your everything to beat a time. When we give that last 10% to go all out, that’s often when we slip into patterns that do not benefit our pelvic floor. Or when we’re tired, heavy and dragging. Keep in mind this is true across the board for all exercise.
Prolapse and Elliptical
- Ellipticals are often touted as the safe option, but I don’t love the handles. They can become a spot to use for hunching over (often seen with people on a stairmaster at the gym) and this can lead to pressure down on the pelvic floor. I usually have success asking women to hold on lightly, just enough for balance, and to come tall by stretching through their torso. This helps a great deal with managing pressure.
The biggest takeaway for cardio that can be applied to anything from rowing to jumping rope is that you have two kinds of forces that put pressure down on the pelvic floor.
#1. Gravity impact force. This is the trampoline, running and jumping.
Leaking with jumping or impact could be more of a nervous system issue, which would cause us to look at the whole of the pelvic floor and check strength, tightness and timing.
#2. Internal pressure management. Due to body positioning, poor abdominal balance, bearing down or generating unmanaged pressure. This can happen anywhere, during any type of movement.
A sneeze, cough, yell, talking with force in a bad position, or sitting/standing with upper ab gripping can generate internal pressure just like lifting something heavy or in an awkward way.
We use different strategies for both these types. I find women will often have issues with one more than the other. (The women who suffer from leaking are nodding their heads now!) I also find that women with prolapse issues will often suffer more (but not always) from pressure leaking issues than impact-related leaking. Which makes sense, since prolapse is a pressure issue.
Will Walking Make Prolapse Worse?
Like we talked about in the above paragraphs, walking might be amazing or it could make you feel worse. A couple of simple things to think about to help make walking more beneficial for your pelvic floor:
- Swing your arms and rotate through your upper body. Staying stiff through your torso can actually generate more pressure.
- Come tall and stretch up slightly through your torso. Think of this as lifting your organs, and just make sure you don’t arch back a lot more to do it. This isn’t military posture, just a little coming tall.
I often find there is a sweet spot to the length of the walk. Too far, and that’s when the prolapse starts to get worse. So keep your walks reasonable, and build up in increments of a half to one mile. Don’t go from nothing to a strenuous 5 mile hike!
Can Jumping on a Trampoline Cause Prolapse?
There would need to be a couple of things going on for jumping on a trampoline to cause or contribute to prolapse. One of those scenarios might be someone newly postpartum.
When you’re early postpartum, you still have quite a bit of ligament laxity. This can make for a lot of organ movement with jumping. To compensate for this, you’d need extremely strong pelvic floor muscles. Pregnancy has been shown to weaken abdominal and pelvic floor muscles, even if you’ve had a c-section. Pelvic floor muscle weakness can occur at other stages in life, but postpartum and during menopause is the most common tie.
The other thing that can contribute to prolapse is if you bear down when absorbing the impact of the rebound; but if that’s your strategy, then you’re probably bearing down at other times in life as well, so it’s all contributing.
Weight Lifting and the Pelvic Floor
Now that’s my favorite question! It’s important to take into account where you are in your diagnosis and training level, but most important is body awareness. The number one thing we want to accomplish as quickly as possible is recognizing the feeling of bearing down. This is the only thing that will cause prolapse to progress and get worse. So the faster you learn how to feel it, the faster you can start improving.
Once a little body awareness is developed and someone can feel if they are bearing down, I want them back to lifting as soon as possible. Not lifting weights decreases muscle mass, which affects bone density and hormones.
As a healthcare provider, I want women working out and I want to get them back to weights as soon as possible!
Bearing down or generating too much pressure is a common strategy most people use when lifting something that’s too heavy. The weaker you get from not lifting weights the heavier things feel in your daily life, and the more you might have to bear down to lift that Costco box into the trunk.
Women often get the recommendation to not lift anything over 10 pounds when diagnosed. Which can be good advice for the first week or two -- but that advice should only last until they get some help with pressure management. You have to be strong to deal with life! But, that said, you want to be smart and systematic about it.
Can Menstrual Cups Cause Prolapse?
Personally, I don’t think so -- but it might make your prolapse more symptomatic, or it might give you support. There was a study looking at prolapse improvement after internal pelvic floor release work that showed all the women had improved prolapse grades and/or symptoms after releasing tight pelvic floor muscles. So we can draw the conclusion that tightness increases prolapse symptoms and grade appearance.
Menstrual cups press out on the wall of the vaginal canal. Some women respond to this pressure by getting tighter. (Some of these women may not respond well to pessaries, either.) I have also heard anecdotal stories of the cup sucking to the cervix, which I think would only be an issue if you pull down without releasing the side of the cup and suction first, but this is something to consider. Menstrual cups can be a great option, so don’t be afraid to try one if you’re curious.
Prolapse is one of the hardest things I’ve ever dealt with, both personally and professionally. There are so many factors that can contribute to healing and improving your prolapse that it makes for a rather complicated issue. I hope you’ll give yourself the gift of a little time and patience, because the hard work will pay off!