Jessica and I found Sarah after our first pregnancies, and this year we conveniently became pregnant a second go around. We had such great success with recovery after the first pregnancies that we thought it would be insightful and interesting for others to follow our journeys after our second ones.
I am an orthopedic physical therapist who had been weightlifting since high school, participated in a lot of yoga, and played competitive women’s ultimate frisbee prior to my first pregnancy. I spent a lot of my free time learning about all things related to muscles and the body. I remained fairly active through weightlifting during my first pregnancy which was a fairly easy pregnancy. I noticed some doming happening with certain exercises which made me eliminate those exercises, but I didn’t fully understand what it was or meant. In PT school, you basically get a day of women’s health where they tell you what a diastasis is (no mention of prolapse) and about leaking or painful sex as issues with the answers being kegels, vaginal weights, and progression of crunches. Then we’d have a women’s health PT to refer women to beyond that. Any time I sought advice on what to do during pregnancy, I was vaguely told to “keep up with whatever you feel like doing based off of your exercise past” and for postpartum it was “just do what feels comfortable.” Well alright then...
At my first daughter’s birth, I ended up needing an episiotomy and vacuum assist due to her heart rate being low, but overall I had no pelvic floor issues right after pregnancy.
I started doing bodyweight exercises after the first month and progressed to weights once I was “cleared” at my 6 week appointment, and I held off on running for about 8 weeks. However, I noticed that my abs contracted in an imbalanced way, with my right side being overly dominant. I had a deep but not wide diastasis that ran almost all of the way down, and I felt generally crooked. My right hip flexor always felt tight and I just felt weird standing on my right leg. Let it also be known that I came into pregnancy with a history of resolved back injury and knee surgery, but residual right hip flexor tightness that I could deal with. At this point I could lift relatively heavy without issues, but it didn’t feel like it was improving anything. I also remember the first time I went back to playing frisbee (6 months postpartum) and as I went to throw a backhand I could tell how I had no power or connection in my core. I occasionally had a heaviness and tampon feeling in my pelvic floor after 2-3 mile runs. I had no leaking or consistent or lasting symptoms, but it got me concerned.
After applying what I knew to my recovery and feeling like something was still off, I somehow stumbled across an article Sarah had written that a friend had posted on Facebook. Now, I am a complete snob and judgey of exercise and advice when it comes to the human body. Incidentally, Sarah and I went to the same graduate school a few years apart but it was her knowledge and emphasis on things that I cued for and taught patients in a similar way that impressed me. She also helped make sense of some things (PRI, aka weird breathing drills) and put them into an applicable and functional context. I was sold.
I purchased Sarah’s diastasis program and joined the Facebook group. The majority of my friends don’t have or want kids, so I was on this adventure on my own. I was blown away with the support in the group, realizing that you are not alone with what you are experiencing, and all the things that go with being postpartum. I had come from a community of ultimate frisbee players who emphasized strength, knowledge, and women empowerment, so it was great to find another parallel environment. Shortly into it, Sarah reached out to me about helping out in the community in trade for free programming. Cool! I went through all of the programs because I’m a nerd and kept finding layers to familiar movements that I hadn’t experienced before. Then I joined her in helping with her continuing ed course, further learning more from here. And now I work part time for Sarah as well as a strength and conditioning coach for a local high school.
I would occasionally roll my eyes and think “yeah right, like this is going to do anything” while working on the program, to then be proven wrong, such as the importance of skin rolling and how 5 minutes of doing it would make my DR go away when I checked it in the beginning. This made me “buy in” even more. I was feeling stronger and my DR was improving. Unfortunately, a few months in, I was playing league ultimate frisbee and while landing on one leg after jumping, I got hit by someone and reinjured a previously replaced ACL (a ligament in my knee). I knew I didn’t want surgery so I didn’t bother getting an MRI, but instead proceeded through Sarah’s programs.
At some point during my journey, I had also developed prolapse. Initially I knew I had pelvic floor tightness and some of the occasional heaviness, tampon feeling I mentioned above as well as air bubbles. I was in denial about it for awhile, so I don’t remember exactly what caused it and it’s all a bit of a blur. I just remember checking one day and seeing that things looked very different than they had freshly postpartum in not a good way. When I realized what had happened, I immediately backed off and paid full attention to the finer details of Sarah’s programs and the infamous breathing, and I backed off on what I was doing otherwise. I have some thoughts as to contributing factors, but don’t think that there was just one thing that did me in. Again, I don’t remember the exact time lines of things, and honestly it could be an accumulation of various things. I also believe it’s more about moving forward and not dwelling on the “could have’s,” should have’s,” “would have’s” of the past.
A year and a half later, after working on cleaning up some cheats and improving the breathing and bracing strategies that I had been able to get away with before pregnancy, I was able to fully return to playing frisbee at league level (the only level I planned on returning to anyway after having a baby, due to time and general age) and in some ways be stronger than I was before with no pelvic floor or knee issues. I did Sarah’s workouts 6-7 days a week, really paying attention to what I was doing, videoing and watching myself, and noticing what I was feeling not only during the workouts, but also after. I thought about breathing throughout the day and also just put my head down to have the best intentions and not beating myself up about all the things I wasn’t doing exactly right. And what do you know, my movement patterns improved with those good intentions rather than with only seeking perfection at that exact moment in time, I got stronger, and my symptoms decreased. I was able to do sets of single leg squat with 25# and accomplished my first pull up. It was great!
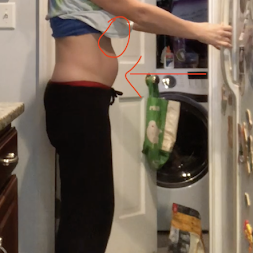
As an example of my improved breathing and bracing, check out the difference between the end of my exhale when I first started vs 6 months later.


Then I became pregnant with baby number two, and that’s where the new intimacy with my pelvic floor and what really happens to your body during pregnancy occurred.
Stay tuned for pregnancy round two...
Anna's Pregnancy Transfotmation
Ah pregnancy...All things considered I get away fairly easy with pregnancy. That being said, I greatly dislike being pregnant and am ready to be done at about 6 weeks, so it feels like a very long 9 months. As my husband says and wanted to make sure I pointed out, I’m a “busy bee.” Exercising is an outlet for me and I really value being strong, so it’s hard to slow down and feel yourself going into a slow regression despite the efforts you put in by showing up to exercise.
Part of what made me so frustrated with pregnancy care the first go around was the lack of information or knowledge out there to let women know what to do (or not to do) activity wise during pregnancy. I know everyone is different, but some better guidelines need to be established to help women learn what to specifically watch out for and monitor during pregnancy.
Sarah had just launched the “Perfect Preggers Workout” series before I became pregnant and I found it to be a great resource through this pregnancy. I probably didn’t watch as much stuff as I could have, but I really valued the trimester expectations that were laid out and the birth prep section. I then felt like I had the knowledge to be able to listen to my body, give myself some grace, and proceed accordingly with what workouts I did. It’s all about understanding the philosophy so you can apply it to whatever you want, vs just renting it and not being able to go “off script.” It was also great to have someone tell me that it was okay to not push myself, that some days I was going to be tired, and overall just to try to stay active and apply good breathing and movements to daily life.
It’s amazing how when the baby is no bigger than a gummy bear, you can already take note of habits and patterns that you’ll have to battle throughout pregnancy. Thanks, hormones! I right away noticed the return of increased pelvic floor tightness and patterns I had worked so hard to get rid of after my first pregnancy such as shallow breathing, tight right hip flexor, and feeling twisted. The good news was this time I wasn’t so far removed that my body didn’t know how to get out of it. I had improved my recognition of the habits so that I could catch onto them right away and had the tools to undo. This ebb and flow happened all throughout pregnancy in a general slow regression as my body changed shape and the baby got bigger. I also had pubic bone and front hip stiffness after any amount of sitting where I felt like I had to slowly get out of a flexed hip position. I could see the contributing movement accomodations and postural changes that occur during pregnancy and how it made sense that postpartum we have to put in a lot of time reconnecting with certain muscles (lower abs, adductors, glute max, and serratus) and reestablish a 360 breathing pattern. I joked that it was like doing muscle CPR to try to keep them alive as long as possible and set myself up that much better postpartum.
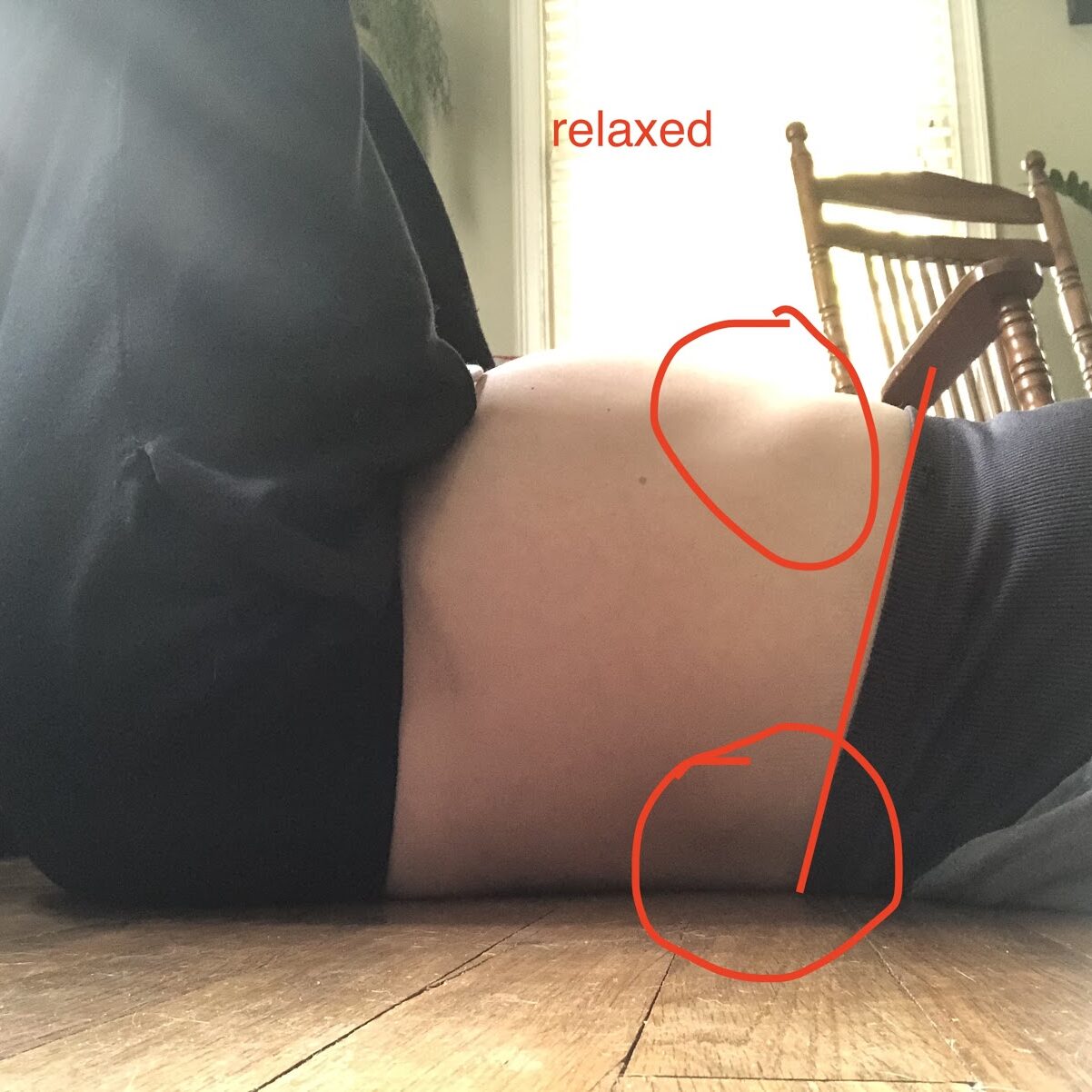
I found as I went through pregnancy, I had to make some positional accommodations during exercises. I had to position myself into more of a flexed posture, or what felt like a posterior pelvic tilt, when I was working on back body expansion. While doing exercises in sidelying I had to prop my head and shoulders while laying on my back to better set myself up for success. My neutral posture progressively became more of an anterior pelvic tilt and swayed back, so I made adjustments to help connect to my muscles and breath. I even noticed how it made sense that my adductors would need some rehabilitation after pregnancy because to accomodate my growing belly and pelvic position changes, my knees had to splay out to the side and hips went into more external rotation as their neutral. I couldn’t correct that movement, but it was fun to observe.
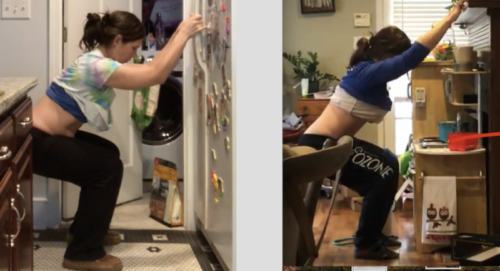
Below you can see posture changes that occur while pregnant. The same pattern existed standing up, but were made more obvious laying down on my back. My rib cage angle was more pointed upward and wider to accommodate the growing belly changes resulting in the increased back arch, which lead to subsequent limited back body expansion and disconnect with my abs.
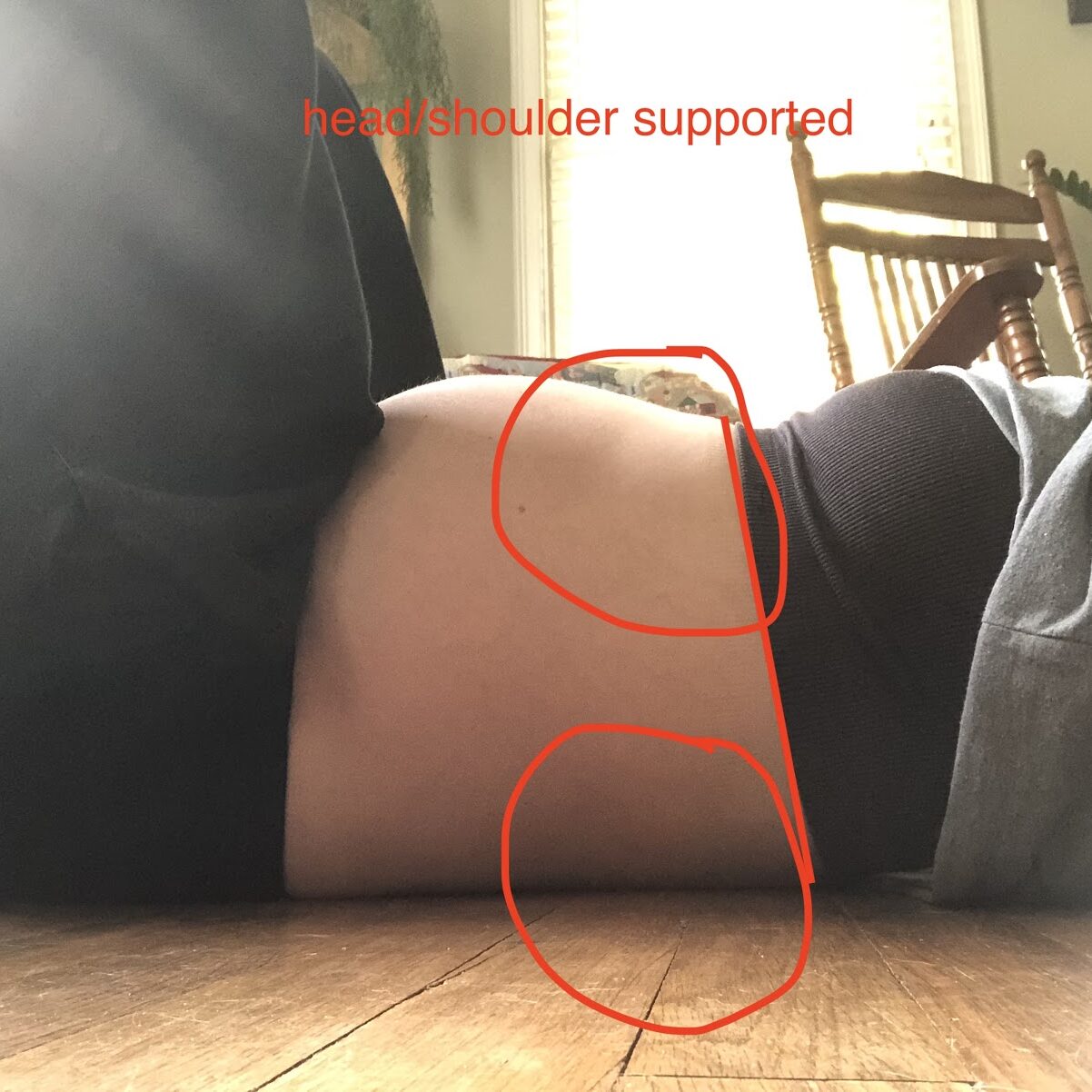
You can see below how the belly gets in the way of being able to flex the lumbar spine no matter how hard I tried, resulting in limited back body expansion and disconnect with abs.

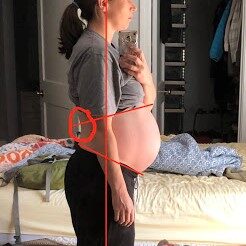
At 25 weeks pregnant you can already see the anterior pelvic tilt and sway back creeping in that becomes more exaggerated at 39 weeks. You can also see the addition of forward head posture and rounded shoulders and a more obvious high hinge point. In my defense, the 39 weeks pregnant picture was taken while I was in the early stages of labor so I was having some increased abdominal tension, I feel like I had looked better than this the day before 🙂

Before every workout, I had to see where my body was at on that specific day. Some days I felt like I was just going backwards, but other days I was able to accomplish something better than I had 2 weeks before because I had spent time listening to my body and cleaning up my movements and breathing patterns. This made it hard to have a complete game plan of what I was going to do. Overall, I continued to lift as much as I could up to 7 months, monitoring doming during activities, pelvic floor symptoms during and after, and pubic bone achiness. Some days I felt great and for the better afterwards, and other days for no apparent rhyme or reason I didn’t. Then I came down with another cold, which wasn’t as bad as the previous one that had lasted for a month, but it resulted in my focusing on more of the “rehab” type exercises that I dubbed “my anti-pregnancy” workout that Jessica shared last week (and will eventually be in the Perfect Preggers Workout). Despite not lifting, I constantly checked in with posture, breathing, and lower ab isolation throughout the day as well as walked 1.5 miles every day with good intention while pushing my daughter’s stroller.
Anna's Labor Story
As I got closer and closer to my due date, I couldn’t wait to be on the other side of pregnancy where my efforts would be moving me in an overall more positive direction again. I also craved the deflated feeling of no longer having a basketball in my belly. Oh, how I looked forward to rounding my back and taking some deep breaths! Only one minor last hurdle….labor.
I was determined to have a different experience than my first go around. I thought I had been in tune with my body before and familiar with breath work through yoga, but over the past 3 years I had taken that knowledge to a new level. I wanted someone who was encouraging to me during the process vs just “let’s get this baby out” and wanted to have options for different positions to be in during labor. So I chose a midwife who worked out of a hospital. When I took my husband to the “meet and greet” and I heard them talk about their passion for the amazingness that women’s bodies are capable of and being promoters of women’s choices, I knew I had chosen the right path. So much of it rang true with what I found in our Facebook group.
My first daughter had been four days early, so I was anticipating that this one (we didn’t know the sex) might come a bit early as well, plus I had been talking to it about how I was ready whenever it was ready. So a week before my due date, I woke up with some contractions. It’s funny how feelings become ingrained in your mind. When I have my period it always comes in the morning so when I woke up that morning with the cramping feeling my first thought was “Oh, I’m getting my period…” only then to remember oh right, that can’t be happening. It’s labor! The contractions were mild and spaced out around every 30 minutes, so I continued about my day and worked from home. However, I felt like maybe it wasn’t wise to go to my strength and conditioning job, so I contacted them about starting maternity leave that day. My husband was a nervous wreck with the unknown of when we’d have to leave for the hospital, but I figured we might as well proceed with our day until it was time.
Around 4:00 pm my contractions began to intensify and increase in frequency. Over the next hour things ramped up quite a bit and started occurring every 5-10 minutes, and I had to stop whatever I was doing during the contraction. I started to focus on maintaining my deep breathing through the pain. I would visualize how each inhale would gently encourage the baby lower and every exhale my pelvic floor would relax and naturally lift back up, but not tighten up. I also focused on not clenching my jaw due to the relationship tension there has with your pelvic floor. This allowed me to have a less threatening place to focus on.
During our 15 minute drive to the hospital, things continued to intensify. When we arrived they took me back to triage to assess me before putting me in a delivery room. However, upon initial examination, the nurse concluded that I was fully dilated and broke my water in the process, so I was not going to be moved anywhere. She didn’t want me to have the baby in the hallway, how thoughtful. My midwife was stuck in traffic, so they brought in the on call doctor. Instead of panicking, I continued to focus on breathing, using Annatina’s tips of exhaling an “O” or “A” sound to help my pelvic floor relax, and just feeling what my body needed, encouraging it to relax as best I could. The midwife arrived before the on call doctor had to take any sort of action.
I could feel my inhales wanting to creep up into my neck as delivery got closer and I kept trying to direct it down instead. The midwife tried to manually help relax my right pelvis and pelvic floor, but I could feel my body recoil and tighten up in response. I appreciated not having an epidural this time around so I could feel what was happening in my body and consciously assist in its effort rather than forcing anything. The baby’s heart rate was lowering and I believe everyone was becoming a bit nervous, so in the end I wasn’t able to fully “breathe the baby out” and had to push. The pushing was done with a held breath after a full inhale instead of an exhale and ended up taking four to six pushes. It was another girl! In the end, between arriving at the hospital and delivering, it all took about 50 minutes.
I ended up having second degree perineal tearing that needed some stitching and first degree urethral perineal tearing that did not need stitching. I was bummed out by that because my goal had been not to tear. I have my theories as to why this happened: I’d had some pelvic floor tightness for the four days leading up to delivery that I had not been able to fully clear up, my pelvic floor response to the well-intentioned manual attempt by the midwife, and my fighting against glute clenching during the contractions and having to push a little before I was fully ready to put that much force into it. But so it was, and I had to tell myself I did the best that I could which was still better than the prior experience.
I had made it through the hurdle of labor and was ready to work toward my recovery, reaping the benefits of the foundations I had laid while recovering from my first and during this pregnancy. Onward and upward!
Anna's Recovery: Week 1 & 2
WEEK 1
While I was pregnant I looked forward to the days when I would no longer have the discomforts of pregnancy, but I knew there would be a transition time swapping out those discomforts for the ones of being freshly postpartum. Things definitely felt stitched together very tightly, and sore to sit. Ice was my best friend and I am really trying to heed the advice of the midwife to focus on taking it really easy for the first 2 weeks. I told my three year old daughter that when that baby first came out, all of mummy’s muscles would be gone so I couldn’t carry her or do as much stuff with her. However, I would get stronger again and be able to do more. She mostly understood and has made several comments about me not having muscles right now, but she has muscles. There was a meltdown one night about me not moving a chair back into her room and she said that she wanted the baby to go back into my belly so I could do it. Ha! She is very much a mama’s girl and creature of habit, so there were lots of things to be tested with daddy doing them instead of me.
One of the first things I did in the hospital was a modified, seated forward fold type action rounding my spine. Oh it felt so good! I had to be gentle to not tuck my hips because I could feel that tug on my stitches, but the breath into my back felt so good. I continued to try and focus on relaxing my jaw, neck, and pelvic floor as I was hanging out in the hospital and I focused on 80-90% of my breath going into my back with just a touch to my pelvic floor, letting everything naturally rebound back up.
I checked my diastasis early on and it was surprisingly not that bad. I didn’t have anything really below my belly button, it was about 2 fingers wide around my belly button, one knuckle deep, and above it was about one finger wide and one knuckle deep but not all of the way to my sternum like it had been my prior pregnancy. My rib angle was greater than 90 degrees which is to be expected with accommodating a baby, and I could feel a bit of the twisted feeling in my pelvis with my left leg feeling longer than my right. I wasn’t greatly concerned about the rib cage angle because research shows that women who close up their diastasis really early end up putting more pressure on their pelvic floor, so it’s a bit of a safety valve for your pressure system and a self limiting factor for activity in the early stages. I was more concerned about how my pelvic floor was going to handle things.
On the fourth day I thought in the morning, “huh, I haven’t cried yet…” Well, I should have known better. My husband had to try and figure out how to handle three ladies crying all at once. That first week is so hard! You hurt, you can’t do anything for yourself (even having to ask my husband to constantly hand me water, which doesn’t have to be far away to be out of reach when you have a baby stuck to your boob), you’re constantly nursing, and my routine and relationship with my first daughter was going to be different. She was no longer the center of my world. It is weird to go from having this little person who can talk and communicate with you and you have a bond with to then be constantly in demand with a baby who doesn’t really give much back to the relationship for the first few months of its life. So, guilt all around.
However, the universe knows, and on the following day I was given a day where the baby slept a bunch and I finally felt like I had some time when I wasn’t holding a baby. All of that cluster feeding over the past few days led to my milk coming in so the baby was more satisfied with the results of her labor. With the increased milk supply, I also felt an increase in hormones in my body and could feel greater ligament laxity. I noticed muscles such as in my neck did tense up a bit to try to provide some stability, but overall it felt great to move around and be able to do simple things for my daughter like get her ready for the day. I continued to focus on taking it easy. My stitches finally felt like things were healing and didn’t feel so swollen. With kids and also with recovery it’s all about everything — the good and the bad — being a phase. When it’s bad you just have to hunker down, do the best that you can do, and know you’ll make it through. And when it’s good, you better enjoy it for all it’s worth and live in the present.
My main focus with recovery during this week was to do gentle breathing and rewire how my pelvic floor functioned with daily activities such as getting up and down from a chair. I mostly inhaled to prepare and then performed about a 5% kegel just to encourage the lift up. Since I am prone to tightness and had the stitches I really didn’t want to fully kegel, but just make sure that at least I wasn’t bearing down. I tried some gentle lower ab engagement just to see, but felt it tug on my pelvic floor so I knew it wasn’t ready for that yet. I also spent time noticing where I was holding tension, which was my right jaw and pelvic floor. I could feel it wanting to clench and repeat the sensation it had from when I was in the end stages of labor or when the midwife tried to assist, particularly during nursing when the latch wasn’t great. Per Gloria’s advice I did some release work on my temples to help encourage things to relax. I thought about trying Gloria’s trauma release drill for my birth, but even though I didn’t feel like it was all that traumatic, my brain just wasn’t quite ready for it yet. I started Annatina’s abdominal massage and used silicone cups in the shower to gently release around my ribs and back to encourage those areas to loosen up so they weren’t restricted anymore from having to counter a pregnant belly.
It’s amazing how in such a short amount of time with simple efforts, you can already see my body transforming:
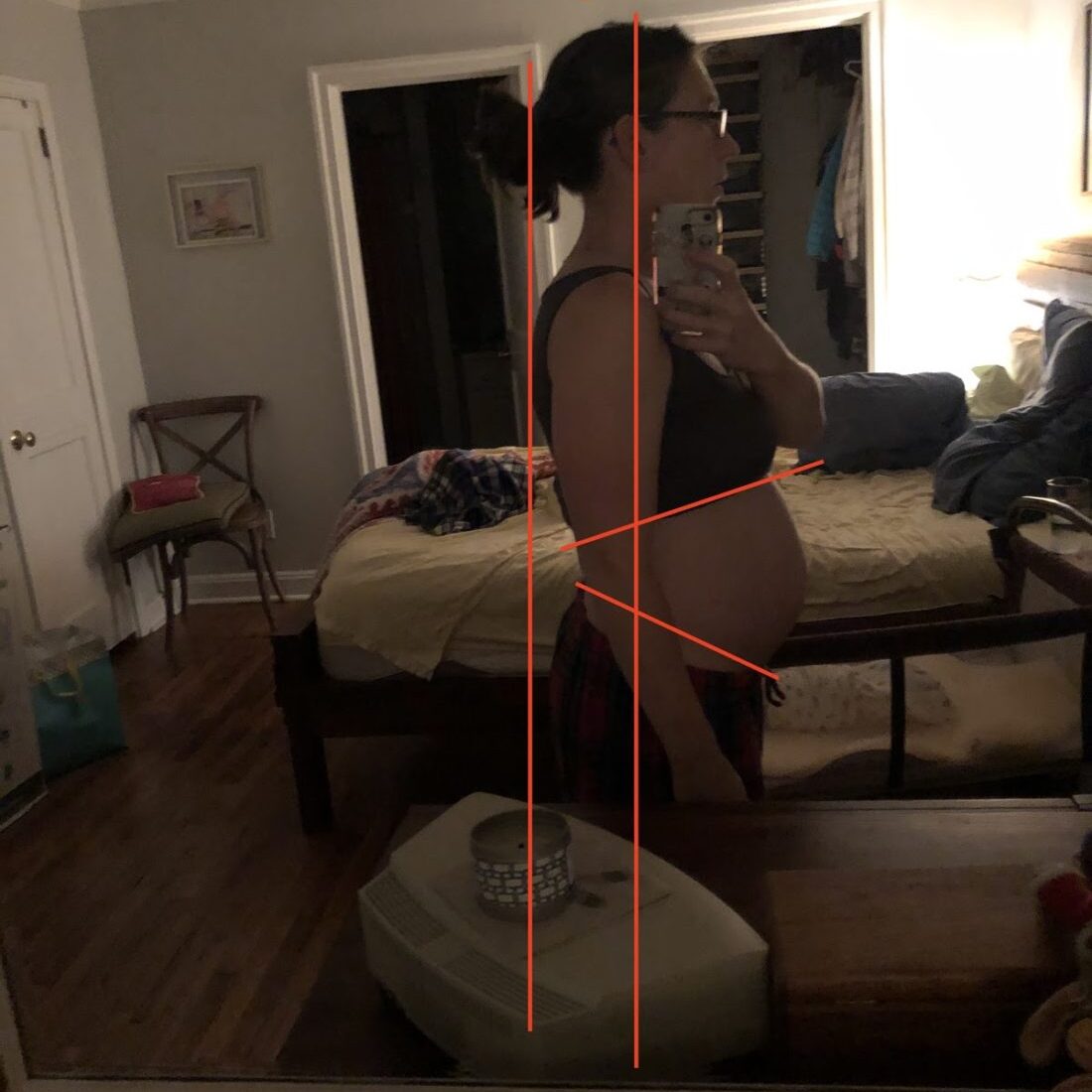

Once that baby comes out, you no longer have a splint for your body to brace against. That’s part of why back-body breathing can be almost more challenging freshly postpartum. While pregnant you might not have been able to breathe well deeply, but your breath didn’t go into your abs much since there was a baby there. Postpartum, the body’s path of least resistance for the inhale is into the abs and most resistance is into the back, which can result in a continued distended abdomen. Yes, I still have a shrinking uterus and belly fat from generalized pregnancy weight gain, but the nurse in the hospital even commented on how quickly my uterus was shrinking and that it must have been my active lifestyle during pregnancy. Go, uterus! In the Day 1 picture you can see how I am leaning back, my upper back would be hitting a wall before my butt. Finally, you can see the other contributing factor of my upward rib position and extreme anterior pelvic tilt.
Now moving forward a week, after focusing on breath work into my back from various positions where I round my spine to support my abs and open up my back plus postural awareness and conscious efforts with daily movement, you can see how overall my posture is better and my belly looks less distended, both of which will improve load on my pelvic floor and diastasis. You can also see that I’m starting to have a bit of forward head posture and rounded shoulders, but that’s to be expected with growing nursing boobs and the time spent nursing and cradling a newborn. You might also see a bit of twist in my left low back from this side shot.
Week 1 win:
Improved posture was the greatest takeaway.
WEEK 2
This week has had more ups and downs. I attempted my first Stronger After Baby 1 workout, trying to focus on not over-engaging anything and simply feeling out movements. It’s so HARD to go slowly. My body wants to move, so once it gets a little taste it’s hard to keep from going full tilt. I was really trying to behave. Afterwards I had some increased pelvic floor soreness, probably from tugging on my still healing incisions despite being mindful and nothing feeling badly at the time. The good news is that the soreness went away the next day, but it told me that I had to continue with the mantra of “less is more” at this stage of the game. This seems so obvious in some ways, but in other ways it feels so gentle compared to even just regular life activities.
I continued to think of other ways that I could mindfully sneak in some strength during daily life. I am continuing to limit picking up my 3 year old and thinking about how I stand up from the ground from a lunge position. I focus on inhaling to prepare, then exhale a little to make sure I’m not bearing down, level my hips as best I can, find both glutes, and switch up which side is first. I am also trying to think about how I stand up from a couch or chair, and I did a few counter squats to help with how I would sit to stand throughout the day.
I started to introduce habit stacking a bit more. During my movement exploration with SAB1 I noticed tightness in my pecs and lats, particularly on my right side. I did a few standing Y’s without the lift just to see what they felt like, and it was like overnight I was down to 75% range of motion. Thanks, nursing boobs. I knew this was going to be a constant battle and important to limit neck pain and improve posture. I tried to habit stack the movement after every time I took a shower (which included some release work and one of the few walls where I could perform this movement). I would do 10 slides as best I could. The movement quickly improved, but I fatigued quickly and I can’t do the lifting off of the wall part yet.
The other thing I focused on habit stacking was the ab challenge of trying to get my lower abs to fire without middle or upper (this was my nemesis the first go around, being a chronic belly button drawer inner). During my previous recovery and during pregnancy I would try to focus on this every time I was done using the bathroom and was in a fully relaxed state. I would stay on the toilet and see how much I could engage my lower abs without anything else, taking a few breaths there. Granted, now I’m always racing to get back to a crying newborn or 3 year old it feels like, so sometimes I forget. However, I try to tell myself that it doesn’t take much time and it’s the frequency of such activities that’s really going to help.
You can see here how my mindfulness and habit stacking added up, and in just a few days my ab engagement improved to include less upper ab gripping. The left is my initial attempt and the right is a few days later. Not perfect, but improving.

On the household front, my older daughter was having swings from being great and helpful to crying because she’s not having her every demand met (ah, the struggles of going from a single child to having a sibling and overall not being spoiled as much), adding to the feelings of being stressed. When I get the baby to nap for longer periods, that time is then filled with seizing the opportunity to do something “normal” with her, whereas when there was just one child it was used for regroup or “me” time. Even the cat and dog were all up in my business requesting their turn for attention. I was starting to feel like I couldn’t get a break or an unstimulated moment.
I was also feeling more anxious about the mess that was progressively accumulating around my house, so I decided to take advantage of a sleeping baby and absent husband and older child to vacuum and tidy up a bit. We have a less than 1200 square foot house, so in theory that’s not asking very much and I even broke it into two time periods due to being interrupted for a feeding. In total I probably did around an hour of tidying up. Initially I could feel my lower abs engage, tried to be mindful about not bearing down, and thought about reaching through my serratus, but the endurance wasn’t there for my lower abs so by the end my back was worn out and I had to lie down. However, that wasn’t the end of the repercussions from that effort.
Then there were the physical adjustments of having a newborn. I was starting to have increased consistency with breast and nipple discomfort and still working on latching such that nursing was causing quite a bit of discomfort. Unfortunately, the seemingly innocent vacuuming put me over the edge in what my body was willing to handle and I came down with achiness and chills. My body was sounding the siren that I needed to address the breastfeeding and continue to slow down. I consulted with my midwife regarding my symptoms and she encouraged me to stay the conservative care course. Yet every latch was becoming progressively more painful, resulting in tears and eventually bleeding nipples and breasts that felt like they were on fire. I could feel my whole body clench in anticipation of nursing and generally felt like my system had tipped into overload.
Over the next few days, I couldn’t dedicate much time to the rehab side of things because I needed to prioritize fixing the breastfeeding situation. I felt like I was in a catch 22 where I had serious engorgement that led to latching issues and increased sensitivity, but I needed to keep flushing out my breasts to get over the engorgement. I ended up pumping and then feeding. However it wasn’t enough milk and my daughter wanted more, so then I made what felt like a heartbreaking choice to supplement with formula. I felt like a failure, but had to remind myself that it was a temporary situation to improve the long haul. The added time of pumping, adjustment time for my daughter to drink from a bottle, and breast care as well as no hands free for feeding with a bottle dramatically reduced even further my time that I could spend with my older daughter, and the increase in her screen time while I took care of everything else added to my feelings of heartbreak. I just had to keep telling myself that this was just a phase and for the greater good. Instead of focusing on the situation that I was in, I needed to direct my efforts on creating a plan and acting upon it to try to take back control. Slowly, over the next few days, my breasts improved. They are still not fully out of the woods, but I am optimistic that this will soon be a thing of the past.
Muscularly, I noticed over the past few days there was a dramatic increase in neck discomfort. There were various contributing factors: the constant looking down to see what was happening with bottle feeding, the increase in stress, the physical pain with nursing that had sent me into fight or flight, and I realized that the pumping bra caused me to fall into a shallow breathing pattern. I focused on release work of my upper ribs and the muscles around my neck and shoulder blades which immediately helped my neck feel better, and I really tried to make double efforts to breathe deeply while pumping and stay aware of when my shoulders wanted to round forward due to either protection or habit. The neck discomfort is still lingering a little bit, but I know that will improve as I continue my release work and am able to incorporate more strengthening activities.
Week 2 win:
Improved top of my squat with improved ability to engage just my lower abs.
Improved overhead reach pattern.
Anna's Recovery: Weeks 3 & 4
Week 3
This was a week of less acute discomfort and tightness in my pelvic floor as well as starting to resume a bit of normal life. I started walking again, taking it easy and feeling things out. First I just went out for a 15 minute walk with the dog, and then as that felt okay I added wearing my daughter. The first thing that jumped out to me was that the second I stepped out of the door I felt immediate pelvic floor heaviness, whereas I hadn’t been feeling that in the house at all. It made me think that it had nothing to do with muscles or breathing, but a state of mind. So the whole walk I tried to trust myself and tell it everything was okay, and tried to see if I was clenching or guarding my pelvic floor. Then I remembered Gloria commenting on “testing” your shoes. I was currently wearing the shoes that had tested well (comparing two new pairs of shoes to each other at the time) during pregnancy, and incidentally had just ordered a new pair of sneakers that were different than the ones I had on. Before the next walk I tested my shoes again and what do you know, the old shoes tested like crap and the new ones were great! I went for a walk again in my new shoes and felt much lighter in my pelvic floor as well as easier to stand taller. I guess that justified my purchase even more! Sometimes it can be the little sneaky things and Gloria’s weird voodoo magic that can help make your battle easier.
I continue to feel tightness on the right side of my pelvic floor where more of my tear and incision are so I started doing some very gentle, depth of a dime, superficial release work. I would have some immediate achiness afterward and just felt some general heebee jeebies about touching my PF after this pregnancy, so I only did it a few times with a day in between. I made sure to be aware of stopping if any feelings of anxiety came up while also telling my body that it was okay. I also started playing with some gentle kegels through iliacus pullbacks, knowing that it always made me feel better before to activate the front of my pelvic floor, while getting the back to relax. I found that I was better able to activate the front, but still had to focus on a subtle contraction and limited reps to make sure I didn’t tighten up too much.
I also played with hands and knees a little bit. Rather than force it, I tried to emphasize “just enough” engagement in my abs, particularly lower, and to work on getting my breath into my back. At first I could feel my back kick in a bit on the exhale, so I had to watch in the mirror for feedback to make sure it didn’t drop during the exhale and lessen my exhale. As I did it a few more times throughout the week, I noticed my back was kicking in less and less and I felt better afterward! However, just like with everything, my main nemesis was keeping my eye out for glute clenching (deep hip external rotators) particularly on my right side. It’s really about jedi mind tricks and being able to engage only as much as I can from the areas that I want without those deep hip external rotators kicking in, and catching myself when glute clenching during the day.
Despite these physical wins and initial optimism of improvements about nursing, toward the end of the week I was becoming progressively more uncomfortable with nursing. Multiple calls to my midwives inquiring about potential mastitis had them telling me to stick with it, but I listened to my body and took matters into my own hands by setting up an appointment with a lactation consultant.
Right away they helped me with latching so that it was immediately improved, but noted that my daughter had some tongue, neck and upper body tightness that was contributing to her struggle. We made an appointment for the end of the week to assess where things were at that point. By that appointment my discomfort had improved some, but I still had some issues with getting the latch “just right” and my daughter wasn’t gaining as much weight as they wanted. They reassessed her latch and concluded that she had a tongue and lip tie that needed to be released, I had developed Raynaud’s in both breasts, and that my supply had diminished. Raynaud’s is the constriction of arteries, and in this case was due to trauma of repetitive compressive forces (aka a bad latch) that results in blanching of your nipples from decreased blood flow and a sensation of pins and needles — or as I’d like to say, “shards of glass into your nipples” — after nursing as well as being affected by cold. Due to this, I was referred to a doctor who would not only treat my daughter’s tongue and lip tie, but also the Raynaud’s. Over the weekend I was instructed to add exercises for my daughter to help loosen up her neck, jaw, face and chest to help with her tongue movement and have a pump-focused plan to help fully empty my breasts and give my healing nipples a break. Talk about time consuming, but it was what it was, and would result in improvement with the bigger picture.
Wins
Beginning to incorporate more normal life things like walking and tolerating it well.
Week 4
I realized the added stress and time spent pumping really affected my posture and breathing. I had more of a distended belly and an obvious high hinge point (sorry I couldn’t make pictures happen). With less time being able to perform my set exercises, I needed to continue to spend time throughout the day thinking about it when I could. It made me realize how it’s so much easier to prevent than undo such tightnesses, and how quickly things could change. However, I couldn’t avoid the causes, so I was stuck with the undoing. That pretty much summed up where my focus was this week. The full exercises and strengthening would be there waiting for me, but right now, my time needed to be focused on breastfeeding.
The pediatrician appointment was great. It felt so nice to be fully heard and to not only help create and facilitate a game plan for my daughter, but for myself as well. You have to love a plan that makes you feel more hopeful about the sucky situation you might be in, no pun intended. He concluded that I had not only developed Raynaud’s, but also developed fissures in my nipples that I needed to focus on healing. I was put on medication both topical and oral for the fissures and Raynaud’s and my daughter had her releases done that day. She was able to nurse right away and it already felt a little bit better for me. I then had to perform two mouth stretches on her 6x/day to ensure that the tissue wouldn’t reattach. This plan was to be implemented for the next two to three weeks which was longer than I had hoped, but at least gave me a time frame to focus on. There was hope that the end of that venture was near!
Then I came home to the older daughter telling me that her tummy didn’t feel well, followed by her throwing up shortly afterwards...
Wins:
Walking feeling better, and starting to become part of my normal life routine again.
Game plan for boobs and feeding!
Anna's Recovery: Weeks 5 & 6
Week 5
My older daughter ended up being out of school for the rest of the week, so it was me and my boobs, my baby daughter and her tongue tie, and the older one with an upset stomach while my husband had to go to work. My mum had come into town to help, but everybody needed and wanted just me. Her main focus was around the house, and I did what I could do for the rest since some of it only I could do, and for other parts I was the only one “allowed” to do it (my oldest..cough cough). This meant my older daughter got more screen time which I hate, but I knew it was just a phase. I concluded there was no point in beating myself up about it and adding even more stress to an already stressful situation I could not control. Plus I acknowledged when I feel like crap from a stomach bug all I want to do is veg out, so I couldn’t really blame her.
I had my follow-up appointment with the boob guy later that week to report some improvement, but the fact that I was still having discomfort made him concerned about a residual underlying infection from mastitis (I told you so, midwives!) and I was also put on an antibiotic. However, my daughter’s tongue and lip looked great.
Needless to say, the majority of my time was not spent toward self-care, and when it was, it was directed toward my boobs (pumping and wound care) rather than my postpartum body. I had to incorporate my other exercises throughout the day and bring awareness to my daily movements, breath, and posture. I took the opportunity of holding my daughter in standing to work on my double leg calf raises with arch focus. I was also having to do more baby wearing to calm the uncomfortable newborn or be able to multi-task and attend to my older daughter.
Breastfeeding and carrying a tiny baby around on its own can contribute to rounded shoulders and tight pecs, and baby wearing pulls your shoulders forward even more. Baby wearing is basically like being pregnant again with a belly that you can occasionally remove, but is also a little more wobbly. I tried to make sure I was conscious of not puffing out my stomach into her or leaning back and to breathe as best as I could, and I focused on standing tall, whether it was in the house or out on a walk. I made sure to use the myofascial release cups on my chest in my shower, even holding it in place as I did a mock doorway pec stretch in the shower. I also tried to pay attention to how I was holding tension in my neck and shoulders while holding and nursing her, as well as in my face and jaw during life in general. I got lots of reps working on lunges, making sure I switched up sides, because it was harder to squat or hip hinge well while having a baby on you.
Despite it all, I felt like my lower abs were coming more on board, and I was proud that when I had an opportunity to check in with exercises it wasn’t as bad as I thought it would be. I started to dabble a little in some more lower ab engagement with a few leg lifts with my feet on the wall, knowing it didn’t have to be perfect to start and that it would be a work in progress. They already felt better than when I first started doing them after my last pregnancy (where it felt like they would never get any better). I started to notice some return of right glute/deep hip external rotator clenching in life as well as during things like hands and knees breathing that I needed to be more aware of and maybe engage a little less. However, I considered it a win that I could feel that so I could actively change it.
I could easily have spiraled into the “why me?!” or “all hope is lost” mode (don’t worry, I had some crying moments), but it was all about marching forward and viewing it all as a phase. You have to do what you can do and focus on what you can achieve at that moment rather than beat yourself up about how you wish things could be.
Sorry for the lack of pictures this week, but hopefully as things calm down I’ll have the time to return to more videos and pictures. It just wasn’t in the cards for these past two weeks.
Wins
Ability to be aware of right glute clenching in hands and knees breathing.
Leg lifts better than where they started after first pregnancy.
Week 6
Well, I am still trying to find my groove. I am noticing that even though I don’t want to get up after the first morning feed, it’s the best time for me to get one pump in and a little bit of exercise. It’s that fine balance between sleep and other forms of self care. Both play their role and are important, but sleep is one that I can fight through lacking a little more because it’s harder to not feel “productive” with it.
This week I feel like I have been countering the effects of being on antibiotics with increased bloating. This has contributed to tightness and lower abs checking out, a reminder of how non muscular things, particularly in our abdomen and gut, can affect our muscles. Right now I can’t control taking the antibiotics, but I can take probiotics and do abdominal massage, and by having awareness in my body, I can know what needs a little extra TLC for tightness and reconnecting with my abs.
The other thing I took note of this week was that it almost felt like I was stuck in inhalation. When working on sidelying breathing, I’m realizing that I focused a lot on the inhale, but on the exhale I could actually keep exhaling if I thought about it. I didn’t have to force the exhale, but encourage it to fully empty the air. The other thing I noticed is that I could feel my diaphragm start to sink into my side as I exhaled, but for the second half my right diaphragm actually puffed out and my external obliques engaged even though it was a relaxed exhale. So I would put a hand there to help it sink in and feel it melt away. It took some conscious effort, but I was able to override. As I did this, I could feel my PF lift up in a relaxed state, which felt great. I like to think of muscles as an accordion or taffy as we want to take them through their full range and “grease the wheels” of the areas that don’t move quite as well.
Despite all of the time I have worked on breathing, how could I still find something that wasn’t quite smooth? Well, I am in “this” currently postpartum body, so I need to connect with that. My body has been dealing with a lot of external stressors, so it’s all about approaching things as a non-biased observer. We can spend so much focus and energy on one component, but by continuing to be watchful, our body will tell us an area that we might have missed or another layer to peel back that’s another piece of the puzzle. We can have a constant dialogue with our body. It is waiting to talk and tell us what it needs if we are willing to listen.
Alright, let’s take a look at posture stuff to take a break from focusing on what I’m battling right now and to appreciate where I have come from:
Here is where I am now compared to one week postpartum. The obvious is how much less my belly is. I still have a slight tendency to lean back and a hinge point, but my hinge point is less sharp, my lean back is a little less, my anterior pelvic tilt is less, my forward head posture is less, and you can see less of an outline of my rectus telling me that my lateral breathing has improved. Overall, I have basically made the curves in my spine less dramatic. Not too bad for pretty much doing only breathing and some assisted squats.

The other thing of interest to note is the importance of using a mirror and pictures for feedback. We can think we are doing something glorious, but then the truth comes out. On the left here is my relaxed posture and the right is my tall posture. You can see that when I think “tall” I actually end up leaning back. Yes, my lower abs flatten, but I also end up gripping more with my upper abs and thrusting my ribs, so I’ll have to play in the mirror and tweak movements to help me rewire what is actually tall. That way when I am thinking about it throughout the day, I’ll know that I’m doing something productive instead of creating new habits.

Wins
Finding the exhale “problem” and being able to rewire it.
Improved relaxed posture.
Anna's Recovery: Weeks 7 & 8
Week 7
Well, this week was filled with ups and downs. I had an appointment at the end of the week to follow up with the lactation consultant, or as I like to call him, “the boob” doctor. I would get a check on my daughter’s weight gain to see what their further thoughts were for heading down the path of more appointments with a GI specialist and see how much longer I had to be on medication for my healing boobs. Needless to say, my mind was still fairly occupied with that, but I was still getting in some basic exercises.
Everything went great at those appointments. Olivia (I guess I should finally tell you her name, as well as my older daughter’s name Adelaide) was gaining weight. I could continue to make dietary changes as needed and keep the doctor’s visit only if I felt like I wanted to go down the medication pathway. Boob doctor said I had to be on meds for another two weeks, but that I was discharged from his care if need be. Woohoo! Then on the way home, I saw a used play kitchen on the curb that I thought Adelaide’s school would like, so I pulled over, picked it up, and put it in the back of my car, which took a little maneuvering.
It wasn’t until I got home that I realized, “oh crap...that was heavy. I shouldn’t have picked that up.” I didn’t have any increase in symptoms, but started beating myself up about it a bit because I had done such a good job of trying to avoid picking up Adelaide and pacing myself with activity. Later that night I felt increased heaviness and ended up doing an internal exam where everything felt lower. I felt defeated. Here I had done all this work and I had made things worse.
I was sad for a day or so, but then kept telling myself that it was still the same path and plan. It’s all about muscle, and muscle can be changed. I then stepped back and assessed what things I could start implementing now to act as a palate cleanser. I realized I had been lying to myself a bit about my meditation game, and I needed to actually do the formal version of laying still and doing nothing for 10 minutes instead of just applying mindfulness throughout the day. I did Annatina’s abdominal massage and PF restoration pose, followed by 10 minutes of meditation focusing on visualizing my pelvic floor relaxing and then being appropriately lifted and supported, while listening to healing frequencies a la Gloria. I also revisited prone glute lifts and being able to isolate glutes before hamstrings. My right side was hamstring-dominant and my left side was accompanied by right side clenching as well. I have a history of impingement on the right side as well as a history of right SIJ pain and nerve pain and had run through all of Happy Hips, but honestly maybe not to the fullest degree, because things were pretty good. However, I continue to have deep right sided tightness, so what better time than when I was already focused on taking it easy and regrouping? Plus, my take is whenever you find something not working well, overworking, or being weak, that’s a reason for your symptoms so you’re holding yourself back if you don’t tackle it.
The following day I felt much better, and continued on my regrouping and assessment of weak links. As the week continued I added in some more exercises, including increased ab strength work, serratus work with foam roller up the wall really thinking about breathing back between my shoulder blades, and thinking about front PF activation with back PF relaxation. With 90-90 I decided to go back to using a wider block and a pillow under my head to keep an eye on deep hip external rotator tightness and open up my back body expansion. I took the idea of breathing back into my shoulder blades from the foam roller up the walls to 90-90 as well. I also started looking at my tibial internal rotation limitations that I get on my right side. When I did that, it’s like my hip exhaled a bit and by the end of the week, my body was feeling more connected and my PF had less heaviness and sticky points. Just making some lemonade out of lemons over here!
The other takeaway with looking back is to actually appreciate how my squat has progressed. I was still badgering myself for not being perfect, but at a quick glance compared to just a few weeks ago, you can see how I have much better length in my torso and glutes from improved core control. I’m so much less...squatty. One of my biggest take aways from my first recovery that I have to keep reminding myself of (and am continually blown away by its effects) was learning to let go of perfectionism. It’s not all about necessarily being perfect, but continuing to chip away with good intentions. I still have work to do, but not too bad.
Win:
Using a setback as a constructive way to identify areas that I needed to clean up and coming out the other side feeling better.
Bottom of squat with more length overall.
Week 8
This week I started off by deciding to join my husband in our walk to go get Adelaide from school while wearing Olivia. Prior to having Olivia, I used to walk Adelaide to school each way and then reduced it to one way as I became more pregnant. I had been progressively increasing my walking distance with good tolerance. However, on this adventure we were running late and had to hustle (probably the first time ever that my husband had to wait on me since I’m a fast walker). With the stress of being late plus the extra jostling, I could immediately feel heaviness in my PF. I told myself that we hadn’t even gone my usual distance and kept trying to be tall and monitor if it was getting any worse. I could basically feel how my hip muscles weren’t ready to take on the shock absorption of a speed walk and my pf was being treated like an unhappy trampoline. There was no change there or the way back. When we got home I immediately sat down, but it was only 2 minutes before Adelaide demanded something, and I realized that my pf already felt better. Just goes to show you to try to not panic when you feel symptoms, but take note and reflect.
A few days later I went to my “6 week” (oops) postpartum check up with my midwife. I had been delaying it some due to logistics with all of my more pressing appointments, but also because I was nervous about the vulnerability of having my pelvic floor checked out. I could feel myself clenching and that things felt worse, and already thinking of my defense about it being tighter these days when she was going to tell me that it looked worse than I had initially thought. However, to my shock she said I didn’t have prolapse but maybe some back wall laxity and that my kegel strength was okay, with it being totally normal for where I was at right now, and that it would keep improving. Umm...what? Granted, I had never been officially diagnosed with prolapse, but from what I could gather I had a certain degree in the front (didn’t think I had any in the back). Prolapse can be tricky to diagnose because it can have variability, and fully assessing takes more than passive palpation, so I felt like her skill set lay elsewhere. All that being said, I do think I was given a sort of mental freedom and elimination of some underlying fear about making things worse and needing to be extra protective of my pelvic floor. I’m still going to move forward mindfully because I still feel like I had some fascial weakness and know I am still vulnerable to do damage.
As the week went on, I started to think a little more about my next exercise step. I felt like my breathing was good and I had internally assessed my kegel to find that it was lifting quite well, so it was about getting stronger and trusting my kegel. I still had some weakness with the coming together part of my lift and my right back side wanted to join the party extra as well as some scar tissue from my incisions, and basically pf muscles feeling like a bunch of guitar strings in there. I looked at MomFit 1 and thought “well, I’ll just run through a few reps and film it to see how things look.”
The next thing I knew, I had completed Momfit 1A. I had taken it fairly easy with heights and weights for things, but felt like everything looked pretty good and certain things like pushups (my right hip flexor hated front planks for so long) felt better than when I started them last time. For the rest of the week, I alternated between the two.
The tricky party wasn’t the execution of the exercises or knowing what to do. It was finding the time to fit it in. Olivia was still working through some reflux so she didn’t nap great or tolerate laying down on her back for very long before gurgling and either choking or spitting up. So my exercises were splattered throughout the day when she was either content hanging out next to me watching or I had suckered her into falling asleep for a few minutes. It was then about having everything set up so that I could jump into action. There is something to be said about the efficiency and relationship between exercises with being able to do them back to back, but I was proud of myself for getting them in and acknowledging on the extra hard days that something is better than nothing. And inevitably, after a hard day, an easier one would unfold to give you hope. By keeping up with stuff in between, it made it that much easier to jump back into things.
I think the best “body ah ha’s” I had this week were working on serratus presses in hands and knees and some further release work. In both the foam roller up the wall and the top of my pushup I noticed I would drop my ribs down and create a lower belly pooch. So with the mirror as my feedback, I practiced the move in hands and knees figuring out what needed to happen to keep my abs and spine intact while just having the movement come from my scapula. Then my abs were on fire. It was glorious. The next time I had to try to figure it out again, but it connected a little faster.
For the release work, I was inspired by Gloria discussing with another group member about applying her depth of a dime release technique to their pectineus. Often we want to smash whatever muscle into submission. I have right TFL overactivity that I’m always monitoring and keeping in check. I foam roll, cup, etc and it’s no longer very effective. Well, one day I decided to try Gloria’s seemingly-too-gentle depth of a dime release (just like I had done to the pyramidalis). And to my delight, as I did it, I could feel my hip exhale with the release taking effect all of the way around my hip into my overactive right glute med. It even helped me perform my left prone glute squeeze without my right one kicking in, and my right TFL no longer stabilized when I was lifting my left leg in the dead bugs with feet on the wall. It was great! Another layer peeled back. Just goes to show you it’s about switching up the strategy and creating a new stimulus to your body so it doesn’t become stuck.
Win:
Starting MomFit! (my chest was even sore from the countertop pushups)
Anna's Recovery: Weeks 9 & 10
Week 9
Let’s just take a moment and acknowledge that the boob and nursing drama was over at this point! I no longer had to be on any type of medication, Olivia was finding her nursing groove to consistently attach better (I could just throw a baby on a boob like it was meant to be!), and I felt like my diet modifications were becoming more natural as well as paying off in her generally be more comfortable. Awesome. Now I could redirect my focus elsewhere.
The main thing I noticed this week was that I was feeling stronger and more connected in daily life things. I was able to go for longer hustled walks without feeling like my PF was bouncing, I was able to lift Adelaide into a grocery cart, and just felt more confident generally with moving around. I didn’t realize how guarded I had been with movements and how some pregnancy tendencies were still with me. I am still making a conscious effort to try to set up good inhales before lifting and not carry Adelaide much (it’s better for all parties since her typical meltdown strategy is “my legs are broken.”)
The one area I did feel like I was pushing a bit was babywearing a heavier baby while cooking with Adelaide in the kitchen. Each individually isn’t insulting to my body, but the combo of a heavier baby, slightly awkward positions while cooking, and trying to keep my cool (aka not clench my jaw and try to let her explore) while Adelaide applies a 3 year old’s skill to cooking. Overall it makes me really happy to be active, but there were some days where I could tell that things down under didn’t appreciate it.
I was feeling better and stronger with the Momfit stuff, catching my cheats and being able to correct them, but I was getting lazier about the unsexy rehab stuff. My body told me it didn’t appreciate that and I could feel some old tightnesses from my previous recovery coming back as well as irritation in the backside of my pelvic floor. It came to a bit of an apex again before I said “okay body, I’m listening,” giving it some foundations and TLC.
I hadn’t fully realized how I had actually gone back to protecting and guarding my PF in fear of injuring it, resulting in a shallow breathing pattern. However, It didn’t feel great on my pf to have a big inhale because it felt like it was all going to the front. Playing around with things a bit, I realized if I initially kept a bit of front PF tension that it helped direct more of the inhale to my back where it was tighter and needed it more. On the flip side, on contraction or lift, my backside, particularly the right, wanted to take over. So I directed the contraction more toward the front as I had done before.
After a live call that Sarah had in the Facebook support group talking about levels of PF contraction, I thought about things a bit more and then took it a step further with working more on the coming together of the sides of my PF and nodding of my clitoris to work more of the superficial layer. I was pretty good at the lift part, but then everything would get involved. Again, it was about not taking a hammer to the situation, but finding the nuance and slowing things down.
From Annatina’s birth prep section, I remember her talking about how the eyes and the PF were connected and I knew that the PF and lower TA’s were connected. After an internal assessment, I had assessed that my PF at 3 o’clock was a bit lacking, so I played with looking to the right with my eyes, working the superficial contraction while doing dead bugs and what do you know...they got better and my right side didn’t bulge out like it normally did. Fun!
Sometimes it’s painful to move slowly and feel things out, but it allowed me to dive into areas that I had been able to fake my way through before. By really slowing down the process and taking these first few months to rewire instead of jumping into the lifting that I could technically do (just with maybe not all the right muscles), I was setting a better foundation for myself to build upon.
Win:
Improved PF control and connection resulting in improved dead bugs aka my arch-nemesis and honestly never fully mastered them last go around.
Week 10
This week was a week of noticing the accumulation of the little things as well as me and Olivia finding our groove. Overall my PF discomfort was feeling better and I was finding better connections with my body. My glute squeezes were still a work in progress, but I was noticing an improvement in them with doing 2x10 of well-intentioned prone glute squeezes every day. They weren’t perfect all of the time, but by consistently chipping away and trying to improve upon them, they were getting better and easier. It really is true that it takes 4-6 weeks to make initial gains in strength and that comes from improving the neuromuscular sequencing and the firing ability of a muscle rather than making muscles bigger. It’s so easy to get sucked into the perfectionist’s game and think what’s the point of doing something unless you can do it perfectly. I had this problem the first go around. It resulted in feeling like a failure, getting sucked into overanalysis, and never really feeling productive, like I got a workout, or like I was moving forward. It wasn’t until I started MomFit last time that I decided to just put my head down and do the prescribed workouts with a few rehab exercises as my warm-up for a month and see what it took me. And what do you know I got better at the exercises, felt happier and more productive, and had improvement in symptoms. I would still take occasional deviations at the end of each month to focus on a certain area and clean up some movements, but overall I would progress.
With taking the first few months of my postpartum journey this time to reconnect and clean up old habits, I helped set myself up for this same plan. Because I was already onto my body’s cheats, I knew a little more of where to look (don’t let my obliques take over and check out my right hip positioning in socket) as well as say “alright, I’ll actually perfect the harder things I chose to ignore a bit last time (like dead bugs and glute, hamstring sequencing) since I felt less pressure to do the bigger movements which also took more set up and time that were harder to sneak in throughout the day.
As I reflect back upon all of this, I realize that things do really improve with intention. My DR is basically gone, my dead bugs/leg lifts feel in better control than they ever did before, and I am able to isolate my glutes lots better than last go around. Before when lifting double leg, I could relatively easily deadlift 130 pounds, but never actually felt glute soreness and sometimes would actually feel my calves be sore instead. I got around it by focusing on single leg work instead but knew I needed to peel back some more layers. Being forced to start back at the beginning this pregnancy allowed me the mental acceptance to start from the foundations again even as I got into the sexier stuff of MF to really work on these foundations. I’m looking forward to seeing where it will take me as I keep getting stronger as a whole because you can only cheat your way for so long until you plateau or an injury happens.
Even though I was feeling pretty good overall, I was still noticing that I was having predominantly right sided PF and hip tightness, particularly with getting into bigger moves like MF that exposed me for my cheats a bit more. I had done the untwisting series before in the past after some other clean up work and had found it helpful. Often the untwisting series can be great, but we don’t all fit into a neat box and with my history of multiple right sided injuries, I had some complexity to my situation. I had tried some of the untwisting moves before in this recovery, but my body wasn’t strong enough or ready for it yet. I just performed a few sets of each move at the capacity that I could do it (say 75% of the weight on my left leg instead of 100%), but I noticed that I had great improvements in my ability to perform the moves and I could feel my right side exhale. I think that was one of my biggest takeaways from PRI stuff was that one sided pain or tightness can be not only due to another area on that side not working well, but the other side of the body not doing its part. Sneaky!
My current programming was walking 30 minutes every day (you’re welcome dog plus it’s just good to get outside to get fresh air and move my eyes around in all directions beyond a computer screen), doing the PRI untwisting series most days, MF 5 days/week, and then some of the other rehab stuff on those days or on their own of mid back rotations, side-lying breathing and rib mobilization if needed, 90-90 breathing, hands and knees breathing, prone glutes lifts, and dead bugs. I was also trying to include some calf raises and hip hikes to start to target those areas. Hip hikes were terrible for me the first go around, but I finally was able to master them and then it was a game-changer. I still think my glute med needs some extra love (activation on the left and releasing/eccentric loading abilities on the right) which makes sense thinking of the sashay hip action (aka hip drop from weakened glute meds) that happens during pregnancy. I also knew that I needed some attention to my arches. Again, last go around I could muscle my way through but I wanted to take the time to give some extra attention here. Overall I have high arches that don’t collapse, but I question how they aren’t collapsing (do I overuse my lateral fascial line or front shin muscles or deep hip external rotators?) or how they might handle higher loads for such things like running or even just walking. My right one was weaker than my left which I think is a contributing factor to my chronic right deep hip external rotator tightness. It’s just a matter of figuring out what strategy was going to work best for me to be consistent with incorporating exercises for it.
The last component that I was including in my rehab was release work. Overall I am not nearly as tight feeling as I was the first go around, so I don’t feel as much of the need to cup, foam roll, or skin roll. My main focus externally is on my pecs (hello breastfeeding) and calves with my cups in the shower or rolling pin for my calves and I’m trying to do a little more on my right hamstring to help give my glutes a chance to win that fight. Otherwise, I’m working on internal release work to my PF (Annatina has some great stuff for this in the guest section of PFP) as well as working on my incisions. I just do a little internal release at a time because it’s easy to get carried away and my body doesn’t like how it feels afterward like it’s too exposed. I find the internal release is also a good assessment of where my body is at and functioning and another way to look at progress. After doing a few days of the untwisting series, I found I had a lot less backside, particularly on the right side, PF tightness.
With all of the work I had been doing on the little things and showing up, I started to notice bigger improvements in my overall daily functional strength. I found I could easily lift Adelaide (35 pounds) into a grocery cart or carry her in from the car after she had passed out, as well as simply thinking less with whatever I was doing in life. So overall my plan was paying off and things were progressing.
Win:
Glute squeezes getting easier.
Overall feeling stronger.
Anna's Recovery: Week 11
Week 11
This week I fully returned to CES work taking on virtual calls and returned to my other job part-time with the plan of next week being the full return. In my other job, I am a strength and conditioning coach for a local high school. During the months of January and May, they have what’s called short term where teachers offer various classes 1-2 hours a day (depending on the class), every day for the month. This was going to be my first time teaching the class and would result in a busier January and May from a work perspective. Good work on my pregnancy timeline planning.
I was tempted to just go ahead and fully return at the 11-week mark but thought my brain and body would appreciate one more week off from the roll of a strength and conditioning coach where I have to demonstrate moves. My short term class was Women’s Health and Wellness, so it was not only about weight lifting and running basics, but also mindset and nutrition. Plus waiting to go back full time would allow me the week to figure out how I’d logistically work everything one more layer at a time.
I had just been thinking about how much better I have been sleeping this postpartum, compared to Adelaide‘s and how I didn’t have much jaw tension. Well then with the return of more work came more stress (even if I didn’t perceive it as bad stress). And with that came tongue thrusting. The weird thing was that I wasn’t pushing my tongue forward but up into the roof of my mouth like it was suctioned. I wouldn't even realize it was happening until I would check-in and then I had to un suction it from the roof of my mouth. One of my meditations where I was doing a body scan I realized how much general tension I held on the right side of my body and started to try to be mindful about it throughout the day. This way I could spend my time preventing rather than on doing.
Otherwise, overall things were feeling pretty good. I was still getting in the same workouts with the added work and enjoying the mental stimulus. I wasn’t thinking about my PF or feeling it at all during everyday life. I had even reached the epitome of rehab exercise where it actually felt like a real workout. I got a sweat on with my muscles quivering and feeling tired at the end of a MF 2 workout. It was glorious and I had a huge grin on my face afterward.
In MF 2, I could tell I still needed to work on my glute firing pattern on the right side. Particularly on the right leg with the single-leg wall squats, but at least now I could make the connection of what was happening and try to correct it. Before it just felt off or I had hip flexor tightness after or I would feel it in my glute med but in a bad way.
Speaking of glutes. No soreness is not always indicative of a good work out, but boy did those single light wall squats work my glutes. The next morning they were both actually sore. Nothing like some sore glutes to let you know when you’re using them in everyday life, such as walking. This was an unanticipated realization since I normally can’t really feel them working when walking, but when sore I definitely knew they were working.
This level of MF did highlight my continued weaknesses. In hands and knees with arm or leg lifts, I could respectively feel my serratus and glute med/TA weakness. I could feel the shifts and lack of perfection, as well as some quivering, and it was going to be easy to negatively talk to myself but I just kept saying “do I the best you can.” One day while exercising with Adelaide around, I even found I had improved shoulder range of motion when she sat on my back. I guess it helped ground me and gave my body some awareness of where it was in space.
I was looking through old videos and looked at the evolution of my dead bugs and rib cage angle. Both were improving but not where I wanted them to be yet. However, I already feel at a better place with my dead bugs now than I ever did before this last pregnancy. Hooray for that!
Wins
Sweating after a workout
Tongue awareness and being given the opportunity to correct
Anna's Recovery: Month 4
Month 4
And then came the full blast of reality. After the first two days, I realized this is what it is like to work full time and be a parent. Exhausting. Every minute seemed booked and my mental gymnastics of all the schedules and to-do lists was exhausting. I had less obvious big blocks of time so it was all about being able to switch gears efficiently and effectively.
I at least was able to be around for all but two of Olivia's feeds so that was nice. However, I definitely felt a bit like nursing lost any amount of intimacy as she was shuffled through as apart of the agenda.
Olivia decided to not take a bottle on the first day and my school work schedule and location were such that it wasn’t that much more of a hassle to come home instead of pump. That still left one feed where she was going to have to take a bottle and I should technically pump. The hard thing was that even though the time block was only a three hour period, the next feeding time was right in the middle and there was no way of being able to take a break to pump. Olivia solved my problem by being on a bottle strike and then I would feed her right when I got home. However, this resulted in an unhappy baby for my husband to care for, was obviously not healthy, and affected the rest of the night’s schedule.
Adelaide was also working through a lot of transitions and taking it out as her own hunger strike at her new school. It was a new school with longer hours so she was now back to taking naps. So on top of added work stress, I also had two hangry children and Adelaide needing some extra TLC as well as her going bananas at bedtime. It was a marathon when I got home of feeding and bedtime. Where whether due to the nature of me being the one with the boobs or of me previously always doing bedtime routine and despite my husband’s best efforts, I was ping-ponging between two kids that both required me to get them to bed. I would finally be free around 10:30 at which point I was exhausted and didn’t know when Olivia would be awake again for another feed.
Amongst this all, I kept trying to tell myself that I needed to make time for me but the schedule was such that if I had a call on the drawn-out drop off mornings, I didn’t get to walk Gus and my time between my other job was limited.
Something had to give and I told myself it would be just for the month of January. I was still being mindful and moving but I was only able to get in one each of MF and two other untwisting series days. Yesterday, when I did my last MF things that had previously been feeling easy, it felt off and I could tell my right hip flexor and pec minor were creeping back in. Where I was able to do the serratus reach before with ten pounds, I was now back to zero on my right side and I could just feel right-sided neck tightness. Some was a result of pushing it too low with pushups, front plank, and serratus press in my workout earlier in the week where I could feel my neck overworking and some was that I still needed some cleanup work to help my bad habits go away and to counter life with a baby.
That also went for the untwisting series. Everything felt like it functioned much better when I did it as a part of my warm-up or first thing in the morning. Sometimes absence makes the heart grow fonder. Even though it felt like I was far out postpartum, in reality, I wasn’t at all. With all of the ligament laxity from hormones and breastfeeding, lots of baby holding and feeding, and sleep deprivation things don’t stick as well as you’d like. I needed a constant application of glue to help me stick together. However I knew as I kept getting stronger, my body would hold the good patterns over the bad.
At the end of January, came the next transition and back to what “regular life” was going to be. Ah, it feels good to have my regular schedule back and Adelaide has found her groove so that stress had been eliminated. Olivia still refused to take a bottle for her one feed, so it was just my poor husband who had to handle that one. We’re making it work though.
Now back to me and my body. I’ve been consistently doing MF 4x/week, still walking every day, and putting on my investigative skills for my continued tightness in my right PF. I have realized a few things. One, my PF has more layers of tightness than I realized. One day when John had taken Adelaide up to his mum’s house, I reviewed some of Annatina’s release videos. I had been doing some internal release (I had taken a break because I needed the mental break from assessing that area) but hadn’t done much superficial release. I revisited that and man did it make a difference. The feeling that I had been having in my full squat of too much on my PF was due to tightness rather than exposure. Yay. Something I could easily tackle, so I set to it to be better about consistently doing release work again.
The other thing I realized, was on a whim one day I did the yoga pose plow (aka how much spinal flexion can you have). I realized that I basically felt completely suffocated, which I took as I was really still lacking in spinal flexion. So I made the decision to be more proactive about rounding my spine, breathing into tight sides, releasing my back, etc throughout the day. This back body tightness would limit my inhale (making it all go belly) as well as put my back into a position to want to engage more on my exhales and with ab work. It’s easy to stay motivated about getting after it for a few days, but unless you make it a habit, you’ll lose your motivation and get distracted by other things in life. I needed to figure out set times that I could make it happen. I’m trying to be more conscious about taking breaks from work and sitting more on the floor in a flexed spine position, but programmed time is important (like after every few responses on FB or after I go to the bathroom or before or after I eat lunch) otherwise it’s easy to kick the can and “do it later.”
Wins:
Peeling back layers to help me keep improving
Improved strength despite a busier work schedule
Anna's Recovery: Month 5
Each month I notice new self-reflections on where I am at and what I am doing (both productively and bad habit wise). I find that thinking of things in terms of months makes how long I might need to focus on something feel less overwhelming, as well as giving my body time to actually make a change. It also allows me to take one item at a time off the list of things I need to work on or explore, rather than trying to do it all at once which isn’t feasible mentally, physically, or from a time capacity standpoint. Often we want change to happen immediately to gratify our efforts, or we make the task of the change so overwhelming and daunting in our head that we’ll never start. I keep reminding myself that it takes 4-6 weeks of consistent work to notice a change, and it’s also about making sure we gently tap the threshold of our body’s ability to “overload” it. More often than not, consistency is more in our head than reality, but just because we think about it all of the time doesn’t mean we are actually doing it. So when I’m feeling frustrated about a change, I try to honestly look back to see if I’m actually putting the work in that I think I’m doing. Usually, I can see that I need to up my game, which allows me to not be frustrated with myself for lack of change and create a better plan for moving forward.
The overload idea is about challenging the body while not overwhelming it. Yes, we need to do something consistently to build upon it, but if we’re always doing the same thing our brain and body become complacent. This reminds me of people who can dominate a step aerobics class with the 2 pound weights that they haven’t changed for a year, and yet are wondering why they never see a difference. On the flip side, people who went to variability training where they did something different every day (I call this exercise ADD or FOMO) don’t give their body an opportunity to build upon what they’ve established. So it’s a stairstep approach of working consistently on something, reflecting when it gets a little easier, and nudging that bar a little further to reach. Then, after you feel like you’ve exhausted the limits of an exercise, you can still attack the muscle but change course to give it a new stimulus with your approach. That’s why I love MomFit. Sarah did a great job of changing certain things, building upon others, but still not neglecting a muscle so that when you went back to a previous move you haven’t done for a while you’re even better at it!
The last thought about overload is that it’s not always clear what overloading actually is for our bodies. Yes, I felt challenged, my stomach was exhausted, and I quivered. However, because my cheaters (back and psoas) are strong, I am able to do challenging things but maybe bypass the muscles that I actually want to be working (read lower abs and deep stabilizing system). So it’s a bit of a dance with dabbling here, seeing how things respond, then redirecting or progressing accordingly. As long as you are doing a nudge instead of a leap you’ll be fine, but that’s not to say that tightness or slight setbacks might not happen. The road to recovery isn’t straight, but it is enlightening. Time and again I tell people how important it is to use their setbacks or response to exercise as information that our body is giving us. It will tell you areas that you need to work on more, and better set you up moving forward. Jessica pointed out a quote I had shared with her and then forgotten about, “it’s not about bouncing back, but about bouncing forward.”
So this month I reflected on ways I could make things a little more challenging, like adding some balloons, serratus press, or more side planks to my routines. I ended up with some tightness that I had to dig into a bit, but overall it went well and I feel stronger at the end of the month. The beauty of realizing this tightness (I would wake up with my back/sides feeling tight but not painful) is that it allowed me to peel back another layer of my body.
I realized that I am a pec minor gripper and use my lats (which I already suspected but was choosing to get away with and ignore…) for my exhales. I also felt a band of tightness in my right EO when I engaged my abs and my right lats felt a band of muscle despite release work. I started tackling it with overhead breathing with reach every day, twice a day when I could and using that same position when doing dead bugs and 90-90 breathing. The concept is to separate what your chest is doing from your ribs (in a sense, pulling you in two different directions of length through muscle activation) so that I wasn’t in such a tug of war of arms/shoulders moving in one direction and taking my ribs with it, ribs coming down and chest coming with it, or external obliques having to pull down extra hard to fight the tightness in my chest. A week of doing this and my abs felt so different and more balanced with their engagement, as well as my back, feeling less tight overall. I was onto something that I knew had held me back before, and I look forward to continuing to explore it.
Wins
Feeling the quivers and fatigue of a workout.
Discovering and improving upon my ab engagement and breathing strategies.
Anna's Recovery: Month 6
And then the COVID-19 lockdown hit. Talk about throwing a wrench into things. We live in a 1100 square foot, two bedroom two bath house. Needless to say, you can always kind of feel the presence of other people. This month was going into uncharted territory from various standpoints, and we had to proceed into it through trial and error. You can always have the best of intentions or even a plan, but sometimes the strategy behind the plan needs some reevaluating. Each week I would reflect upon the previous week and figure out how to begin again.
We are fortunate that my husband had already decided to be a stay-at-home dad after I had Olivia and I was able to maintain full time employment through my jobs. The problem was that me being in the house felt to Adelaide like having a plate of cookies out all day while not being allowed to have any. It was exhausting for all parties. Then we came up with our genius plan to level out the camper van in our driveway, and poof! The first day I went to work in there and felt the quiet, my brain and body immediately exhaled at being able to focus again.
As I read through the Facebook feeds and reflected upon my own symptoms and discomfort, again and again there were incidences of neck, upper back, and low back pain and the one common denominator through it all… stress. Everyone had gone into survival mode to figure out how to make it through this lockdown time. However, it slowly became a greater realization that this situation wasn’t going to go away any time soon. Just like anything, we needed to figure out how to move from a survival strategy to a more sustainable one, because just surviving wasn’t going to cut it.
I like to think of all of us as having a stress bucket. There can be good types of stress (like hard workouts) and not so good types of stress. No matter what type it is, the bucket doesn't differentiate between one or another. Once it’s full, it’s full. Survival mode made that bucket overflow. It’s important to take a moment to step back and then categorize the stress into what is controllable and not controllable. By realizing what is out of our control, we can work to let go of that stress because trying to change it or focus on it is only going to cause more stress, and our efforts won’t be productive. We can then direct our attention to what we CAN control, which will be far more productive. The stress that we can control will be addressed by how we react to it and how we can change it. One of the stresses we can control is intensity and type of exercise. Even though it might be something that we want, we have to recognize when our body is at capacity and already exhausted in the fight or flight response from the other stressors. So instead of pushing into intense exercises, this is a great time to do our body a better service by working on things that help us ramp down and unwind (like more release work, or breathing drills, or fine-tuning exercises) and find ways to boost our happiness.
I could feel all of this new life’s stress and anxiety building up in my body. I was still working through continued PF tightness (symptoms of trapped gas and bathroom urgency) as well as an episode of tight rhomboid and forward head posture tension. I needed to give these areas some extra love and attention. If I just tried to continue to smash forward my body would rebel, and those issues would be magnified until I would listen. I worked on more external and internal PF release work. I consistently released my serratus, lats, posterior cuff, pec, and neck fascia. I went back to revisiting rewiring patterns of serratus over pec, and if my middle and lower traps were working instead of my paraspinals, lats, pec, and rotator cuff.
I explored why my pelvic floor was tight, concluding that the right side was tighter because of femur positioning in the socket plus the left side was weaker, so the right had to do double duty (the layers of it all.) I revisited prone glute squeezes and adductor strength in functional activities. Adductors fired well and equally lying down, but I could feel how even though I could pass the eyeball test with an upright movement, when I touched with my hands I had to consciously work to get the left adductor to kick in. I checked back in with rotating warriors that I had tried intermittently leading up to this point, since they had been a great help in my last recovery. Previously, I could tell I wasn’t strong enough in some of my foundations of lower ab and hip strength even though once again I could make the movement happen, but the question was, with what? However, now with focused effort and visualization, I could make the right things do the work and felt better for it afterward.
I always say our body will tell us what it needs. We just have to be willing to listen. At first it will start off as a whisper, and if we choose not to listen to it, it will increase to a scream. As we continue to turn inward to listen, we’ll get better at being able to catch on to the whisper rather than having to wait to be clubbed over the head with the message. Taking this time to not only undo but also reflect on the “why’s” of what led me to the tightness would help me take this detour or pit stop while still progressing forward. It was tempting to just keep getting it done and going through my workouts as I started to add in Live Call workouts for the school that I work for, with every workout feeling rushed or always working out with a supervising almost-4-year-old constantly asking “why” or wanting help with “her exercise.” It was all very ramped up and stimulus overload. I had to find what exercises worked for me in this time, find the extra time to do the release work (hanging out on the floor with kids is a great time for foam rolling), and try to pay attention to what extra tension I might be holding while doing my exercise. Often I look to my jaw and how my face is holding tension because it’s the easiest thing to feel. This goes for workouts but also with how I’m handling chirping children. Again, focusing on the stress and tension that you can control and your reaction so that you can stay one step ahead instead of always having to undo that tension. As a wise princess once said, “Let it go…”
Even though this month has been exhausting and the end of it is not in sight, I have had some good takeaways from it that I’ll continue to be able to use moving forward. It’s easy to say “once we get through x, y, or z, it will all be fine.” However, in reality, there will always be some new unknown stress around the corner. Granted, some will be larger and longer than others and some will be harder to control than others, but how it affects us is all about how we respond to the stress. We just have to learn to ride the wave of life and recovery. It will have ups and downs, maybe some sideways and backward action, but overall we have to learn to take it in stride and figure out how to keep our general momentum moving us forward.
Wins
Being able to “begin again” each week to figure out what will work best to move forward.
Identifying functional left adductor weakness so I can work on it and strengthen it.
Anna's Recovery
1 Week to 6 Months Postpartum Summary
Anna's Summary
And here we are 6 months postpartum. I’ve come a long way in just how I feel tolerating everyday life of being a mom let alone taking on leading online Zoom workouts for my other job. I no longer think about what I’m doing when I go to pick up my 3 ½-year-old, throw her around, and can chase her. I am just straight up trusting my body more and thinking less. I still have room to improve and have to battle the increased ligament laxity from breastfeeding hormones and posture effects of nursing and carrying a little one as well as increased online work, but the overall trajectory is upward. Here you can see how I still have some forward head posture, rib flare, and anterior pelvic tilt, but I have taken the extremes of the curves out of my spine and pulled myself upright a bit more. You can see my hinge point is less dramatic and I have less rounding in my thoracic spine. I still am working through backside pelvic floor tightness, particularly the right side, and some intermittent neck discomfort, but feel like I have the tools to keep fighting the good fight. It’s definitely been more challenging fitting it in with this new norm of not only two kids, but the state of lack of alone time right now. However, it’s not changing any time soon, so better off creating a new plan of attack for this than reminiscing on how things once were. I’ll be missing from blog posts, but not missing from putting the work in behind the scenes in not only the workouts but also daily life habits and patterns.
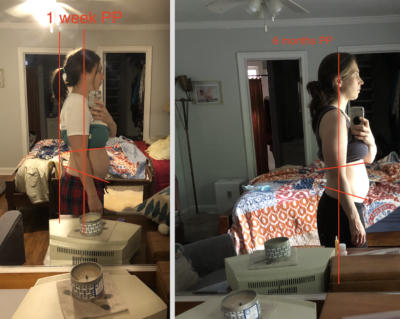
Anna's Recovery: One Year Update
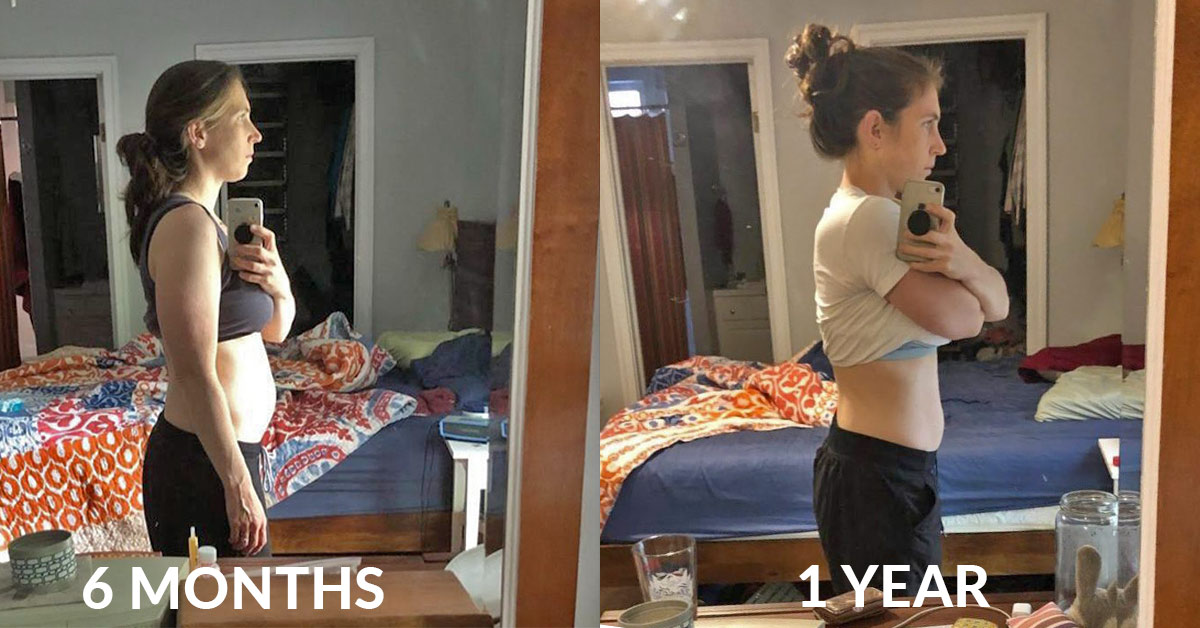
Well – here we are. Barely knowing what day it is, it’s no shock that the one-year mark has snuck up on me, and I can’t believe I’m here. Just a little bit has changed since a year ago, and the day before Olivia’s birthday I did reflect on, “Wow, I’m so happy to be where I am now vs. where I was then – aka, very pregnant.” There have been many ebbs and flows in this journey, from feeling progress to then peeling back another layer and feeling like I’m not getting anywhere. However, the icing on the cake and representation of some hard work was when I was able to do with ease 3 jump pullups right around my one year mark, despite not having worked on any pullups in 3 months. I’m still drooling for the feeling I had 2 years postpartum with Adelaide when I had shocked myself and accidentally levitated up in my first pullup ever (never accomplished even before children), but there’s already an increased ease and balance in those 3 jump pullups compared to before. So, how did I get to this point? What have I been doing in the past 6 months? Well, I’ll tell you 🙂
I am a firm believer in everything in life having seasons. That includes exercise. If you think about it, all professional athletes have seasons (part of why I loved playing ultimate frisbee competitively is that it naturally gave me the season and my “why” for lifting weights). Athletes aren’t going full tilt with the same stuff all the time. As a “recreational” worker-outer, it’s hard to not just go-go-go and have the mindset that time off from your set plan or track will be detrimental to your overall progress. However, I’ve realized that building in some changes of focus or intensities helps with the overall marathon that is life and exercise. I think it’s also about viewing exercise and movement as a lifestyle, rather than a phase. It allows you to enjoy the movement, the exploration, and the journey as well as take the stress off of yourself for times when you might need to reboot or are lacking energy to go heavier for workouts. If you always have the mindset of “go big or go home,” then you’re just setting yourself up for disappointment and not realizing the gains and benefits from other work. That being said, I think it’s also important to realize when you’ve been in the “off” season for a little too long, and maybe it might be time to push yourself a bit out of your comfort zone, get out of your head (stop getting stuck in the rehab loop/picking yourself apart), or figure out how to make more time if it’s always “oh I’ll have more time after I get through (enter phase of life you’re dealing with).” Life is always going to be busy, so if you’re always feeling that you’re pushing exercise to the side or even just doing the “fun stuff” and not analyzing how you’re doing it, then maybe you need to reassess your priorities – especially if you aren’t making the progress you are wishing to make.
The first chunk of these past six months, I was still a bit in a get-it-done mode. I tried to reward myself with the feeling of accomplishment of getting a solid workout done in my smaller than ideal time frame. That meant there wasn’t a ton of time for assessment and analysis beyond in-the-moment thinking (aka, no videoing or mirrors due to requiring extra time to set up). Things were going fairly well, but I was still having occasional rhomboid/neck crankiness (typically timed with theoretical hormone shifts, since I still don’t have my period back) and some PF tightness. I then had a few series of events that brought me back down to reality and forced me to peel back some more layers and assess:
- I took a video of some assisted pullups to help members out with seeing something. I was then discussing it with Sarah, at which point she pointed out that I wasn’t actually using my lats at all… no wonder why they were so hard! This started my detailed assessment (aka, shock and horror as to what was actually happening) into my shoulders. I had already been doing some serratus stuff and had previously worked on lower trap things, but I’m blaming continued breastfeeding, baby carrying, and computer work for not being enough to counterbalance the rounded position my shoulders went towards.
- I kicked a toy train box with my pinky toe. Within two hours, I felt the entire ripple effect throughout my entire lower body to avoid putting weight through that side of my left foot, and so I dove into learning more about arches and feet through Gary Ward’s foot course. I already knew I had things to further explore, but it was easy to put it on the back burner. His course allowed me to take extra time for a few days to assess my feet and understand the foundations of the movements, to then apply them as I went through other lower body strengthening exercises for a positive change in my hips that I couldn’t figure out how to make happen otherwise. (Nothing like living it to learn it?)
- We came up to my mother-in-law’s house for a few weeks, which meant I didn’t have as much exercise equipment or the same set up available to me. This forced me to dive into refinement of movements and turn inward instead. I came upon Katie St. Claire’s lumbo-pelvis course that had slight variations to PRI oldies but goodies. It further supported the idea of how our bodies need that slight increase in challenge to a movement to perk ourselves up and peel back another layer of opening and stability. It became my new morning routine to spend 15-20 minutes working through some breathing drills that helped improve my posture and core. With maybe a few pounds of weight loss as well, you can see below the effects of improved alignment (hinge point has moments of being gone) helping with muscle function, resting tone, and increased ease of tall posture. There is still work to be done and I basically feel like I have to fall forward in my tall posture, but not too shabby if I do say so myself.
I was concerned that I had gotten sucked into the rehab rabbit hole and needed to make sure I was getting back to doing some bigger movements, so I came up with two workouts that I wrote down on a white board. It’s shocking how doing such a small task of writing it down/taking away the mental work of having to remember or that extra minute to pull it up on your phone, etc really helps set you up for more success. The other thing I did was have a morning routine (as I mentioned above) to work on some breathing and also a rehab exercise like serratus press that I could do without feeling rushed/eager to get onto the next thing and be consistent about. This made me feel more ready to dive into my workout in the afternoon, because I had the mindset of basically already being 15 minutes into my workout before I even started. Accomplishing that in the morning allowed me to start the day feeling centered and successful, as well as not making up excuses to push it to the side or get in “just one more” work thing first. I’m also one who does better with a set time to do exercises vs incorporating them throughout my day, because I benefit from finding my groove. My afternoon workouts would include some isolated movements like Ys and clamshells, but I also made sure to have bigger movements like lunges and overhead presses.
When I got back to my house again, I had a band set up on my pullup bar so I could knock out lat and lower trap work in 10-15 minutes when Olivia and I were hanging out in the morning. I also started doing abdominal massage consistently in my early morning hours while hanging out with Olivia, which helped with some urge incontinence feelings I had randomly experienced (after a week of doing it, it almost completely resolved, and now it’s not there). I continued to explore other areas of release work, using various strategies (again, consistency but also novel stimulus helps your body continue to unfold) in my lats, pecs, adductors, calves, and hamstrings, remembering that a muscle can be long or short and have knots in it which will limit its function. I also started including more focused eccentric work to “iron out” the knots and help those muscles become long and strong, have a place to contract back and shorten from, and assist function of opposing muscles (aka, chest presses to help middle and lower trap function).
When I had more time for my afternoon workouts, I’d explore a bit more with movements to help improve efficiency and impact during my next workout. Some days it didn’t feel like I was making strength gains and I questioned if I was making progress, so I made sure I was finding that edge of challenge while still being focused and making sure I wasn’t just muscling through the movements. I would have a week here and there where I just felt exhausted from life. I kept my morning routine, but some days I would then opt to go for a walk or make sure I said “yes” when Adelaide wanted me to run or hop or have a dance off. I think of this as happiness boosting movements, and how it’s so important to make sure that we still play in life as we get older. It was also fun to have moments of athletic coordination that were spontaneous vs rigid, which strength workouts can sometimes fall into. Three months into this, I could see my random jump pullups and exercise that seemed like small, “is this even a workout/am I pushing myself enough?” work was paying off.
It’s all about buying in for the long term development and process, but also making sure you have those mini wins along the way to help motivate you to keep going.
No matter where you are in the process, it’s about movement being a part of our everyday life and touching base with your body, what it’s feeling, and what it’s needing. It will tell you what you need if you’re willing to listen to it, and by reaching out to it one way or another each day, you’ll keep the conversation going and form a better bond with it. We only have one body, and just like any close relationship there can be ups and downs, laughs and cries, but it’s important to keep putting in the work and overall have a positive relationship with it. We can control our mindset and our muscles, even if some days it feels like that’s not the case, so we might as well focus our attention there to get the most out of it and enjoy the process along the way. So here I am, a year out, with some great gains having been made, but also a journey still ahead of me as I keep peeling back the layers. I remember thinking last go around that around 2 years postpartum I felt like myself, without having to think about random muscle tightness or tweaks or imbalances, so that’s the time frame I’m setting myself up with. However, I know that this go around has had different hurdles (mentally, physically, nutritionally, and emotionally), two children, and I’m still breastfeeding, so it’s a soft finish line giving myself a goal to focus on while also making sure to give myself grace that each time comes with different circumstances. Either way, here’s to learning more about my body – and even though there might be some curse words and moments of frustration, trying to enjoy the learning and growth process to become the best version of myself.

