What does your pelvic floor have to do with the strength of your abs? Should you strengthen your abs to help your pelvic floor, or should you strengthen your pelvic floor to help your abs? Should you work on your diastasis to help pelvic organ prolapse or leaking? Does working on your abs hurt your pelvic floor recovery?
Well, the answer is maybe…
Let’s take a look at a few different scenarios where one approach is clearly better than the other and figure out where you might fit! Let’s look at pelvic floor weakness, tightness, lower belly pooching and diastasis, and the best way to address each situation for the fastest recovery!
#1. Will working on a diastasis help heal pelvic organ prolapse, leaking and other pelvic floor issues?
Working on your diastasis might not help your pelvic floor and in some cases may actually make it worse. I see this specifically in newly postpartum women who put more focus on recovering their abs than their pelvic floor postpartum. I also see this with later postpartum women who are trying to resolve pelvic floor issues. Their abs get stronger than their pelvic floor can handle. Our system is all about balance. We have to equalize the effort created by a force (for example lifting the carseat, or doing a crunch) all over our entire torso. If one area is significantly weaker than the other, excessive force in that area can create harm.
A study from 2017 looking at women with a diastasis and pelvic floor dysfunction showed that women WITH a diastasis recti actually had MORE pelvic floor muscle strength (not less) and that women who closed their diastasis faster at 6 weeks postpartum were MORE likely to have pelvic organ prolapse.1 So maybe having a diastasis postpartum actually acts as a protective effect for the pelvic floor?
It makes sense when we think about it from a force perspective and the vulnerability of both the abs and the pelvic floor postpartum. The fascia stretches and gives to help prepare for birth. Did you know 100% of women have a diastasis at the end of pregnancy?2 So the question then becomes why do some women heal while others don’t, and how does having a diastasis create a protective effect against pelvic organ prolapse?
This definitely explains why I see patients who work on their diastasis and end up worsening prolapse and pelvic floor issues.
It brings us back to balance in the system. Let’s dive in and look a bit further.
#2. Diastasis. Why is depth important?
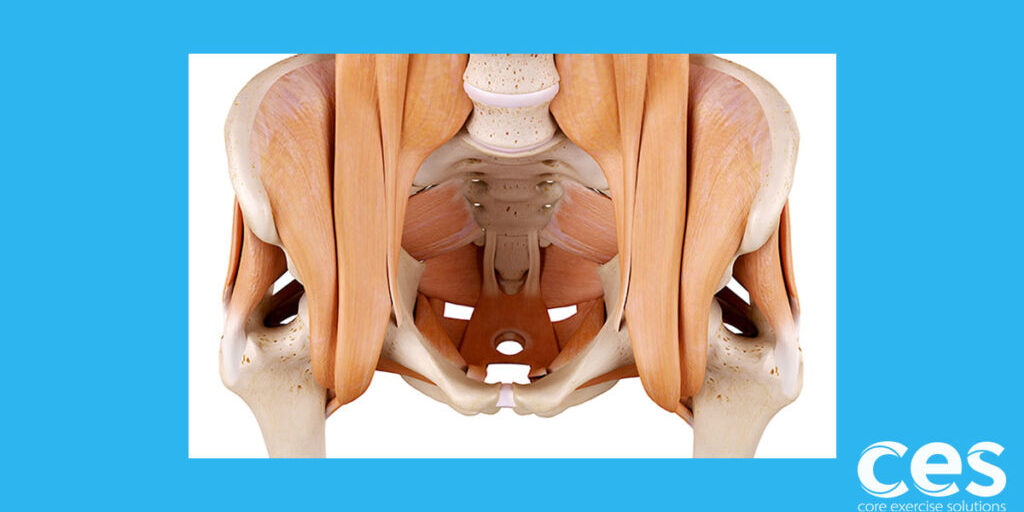
The transverse abdominals (TAs), our deepest abdominals, control depth of the diastasis, and the rectus abdominis (6 pack muscle) in the front control width. The TAs wrap around and form a corset, helping to support the back. The rectus runs up and down the front and is more of a mover or decelerator than a stabilizer. It works to counter the powerful extension effects of the paraspinal muscles, so it doesn’t have the same protective effects for the spine as the deeper stabilizers do.
In other words, you’d rather have a wider diastasis that’s firm than a narrower one that’s deep. Being rectus dominant is like being quad dominant. We need strong quads, but if they run the show with no balance from the glutes or hamstrings, then it increases the risk of knee and hip pain.
One great way to decrease the gap, since everyone seems more worried about that than depth, is to do crunches activating the rectus. The issue is that crunches can be either harmless for the pelvic floor or they can be done in a way that generates a whole lot of force down on the pelvic floor. This could increase the risk of pelvic floor dysfunction. It’s all in the execution of the exercise.
Full-on speculating here - Maybe the women who are able to decrease their gap faster and generate a lot of core tension (good tension helps fascia heal) end up doing so at the expense of their pelvic floor (or at least the ones that end up with increased prolapse as a result).
Hey, I’m not pointing fingers! I’m one of the ones in this boat. It’s taken considerable mental effort for me to re-train how my core loads in order to heal my prolapse. Generating tension was never an issue, it was how I was going about it that was. This is what makes me beg for better postpartum programs. A little education can go a long way toward prevention.
Ok, more on how abdominal strength affects the pelvic floor but first, a quick video on how to check depth and properly contract your abdominals.
#3. Does a lower belly pooch decrease max pelvic floor strength?
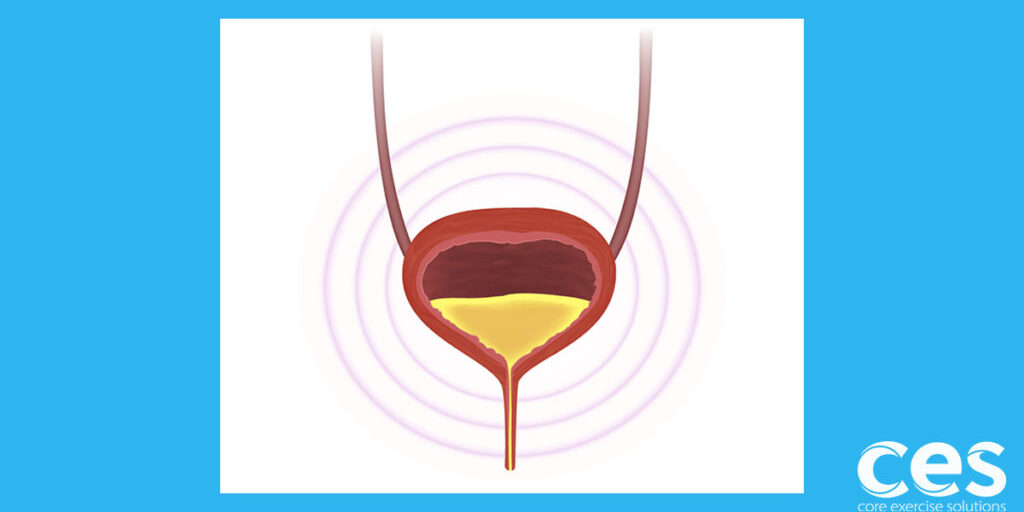
So, this can be a bit chicken and egg. The pelvic floor should be the first to activate when we need our abs and pelvic floor to kick in. But, after that initial contraction, the abs help the pelvic floor continue to fire, fully maxing out a pelvic floor contraction. Try lifting your pelvic floor as hard as you can without your abs contracting. Someone somewhere can probably do it but most of us mere mortals find it impossible because our abs work with our pelvic floor. As a matter a fact, the last 30% of a max pelvic floor contraction is coming from the help of your abs.3 Pretty cool huh?
So in this case, a lower belly pooch could be a sign of pelvic floor weakness, but not always. It’s definitely something to take a closer look at while exploring the best approach, and this would be a great example of when working your core could help your pelvic floor! So, ab exercises are back on the table. (I know I just spent some time in the first section bashing them but all’s fare in rehab and exercise.)
#4. Does having stronger abdominals help with pelvic floor tightness?
Many women have pelvic floor tightness. This is especially true for those women who try kegels but they don’t seem to help. (In some cases, it makes them much worse.)
So, where does working the abs fit in?
The pelvic floor is the master compensator. It will hold tightness compensating for weak glute muscles and it will also hold tightness or overwork compensating for weak abs. See, the pelvic floor plays a huge role in pelvic stability. So every time you take a step, your pelvic floor fires to stabilize your pelvis. When everyone is equally doing their share, which includes the abdominals, the pelvic floor doesn’t have to overwork to provide stability. A pelvic floor that’s working too hard to provide stability can’t stop leaks and it can’t hold up pelvic organs in the efficient manner it was designed to do.
It’s a pretty cool system! So in this case, getting stronger everywhere, including abs, can really help the pelvic floor let go so it can focus on those other important roles.
Note, that I didn't say holding in. When you hold in your abs all day, this can cause pelvic floor tightness and dysfunction. I'm simply talking about becoming stronger in a functional contract and relax kind of way.
So, there you have it. Should you do more ab work? The answer is maybe! 😉 I know, frustrating, but I do know what needs to happen first is establishing the basics. Understand how your pelvic floor works with your diaphragm, master a deep breathing pattern that’s not all belly and establish a mental connection with your pelvic floor so you know whether or not you’re bearing down for exercises. Build a great base in all areas- a mind-body connection, knowledge and physical strength. Once you have all of these, then you’ll start to see a life without worry in your future and endless possibilities.
Want to learn how to help women efficiently heal their pelvic floor and core? Awesome! The info from this article was pulled straight from the Postpartum Corrective Exercise Specialist course where we go in-depth looking at posture, the pelvic floor, diastasis, SI joint pain, back pain and much more. This course is for Personal Trainers, Pilates instructors and Yoga instructors who want to learn new exercises and hone their skills of proper exercise execution. It’s also for Physical Therapists and Chiropractors who want to learn more about women’s health and the most effective exercises to give their patients.
For more info on the course: click here! Looking forward to learning together.
References:
- Bø K, et al. Pelvic floor muscle function, pelvic floor dysfunction and diastasis recti abdominis: Prospective cohort study. Neurourol Urodyn. 2017.
- Patrícia Gonçalves Fernandes, Augusto Gil Brites Andrade. Prevalence and risk factors of diastasis recti abdominis from late pregnancy to 6 months postpartum, and relationship with lumbo-pelvic pain. Manual Therapy. Volume 20, Issue 1, February 2015. 200-205.
- Madill SJ, McLean L. Relationship between abdominal and pelvic floor muscle activation and intravaginal pressure during pelvic floor muscle contractions in healthy continent women. Neurourol Urodyn. 2006;25(7):722-30.
Free Pelvic Floor Educational Series
Dr. Sarah Duvall, PT, DPT, CPT and the CES Team have helped thousands of women create the strength and stability needed to overcome common and not-so-common pelvic floor issues.
Join us today for this 4-part Pelvic Floor Video Series, absolutely free.
We don't spam or give your information to any third parties. View our Terms of Use and Privacy Policy.
Having trouble signing up? Click here

Related Articles
- « Previous
- 1
- …
- 3
- 4
- 5